All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
Impact of GvHD on post-transplantation outcomes following CBT and PTCy-haplo-HCT for adult AML
For patients with acute myeloid leukemia (AML) without a human leukocyte antigen (HLA)-matched related or unrelated adult donor, alternative donor hematopoietic cell transplantation (HCT) from an unrelated cord blood or haploidentical-related donor remains an option.1 However, it is unclear whether the prognostic effect of graft-versus-host disease (GvHD) on post-transplantation outcomes differs between recipients of single-unit cord blood transplantation (CBT) and recipients of haploidentical HCT using post-transplantation cyclophosphamide (PTCy-haplo-HCT) for AML.1
Here, we summarize a recent article published by Konuma et al.1 in Transplantation and Cellular Therapy that evaluated the impact of GvHD on post-transplantation outcomes after CBT and PTCy-haplo-HCT for adult AML.
Methods
This retrospective study was conducted using data from Transplant Registry Unified Management Program (TRUMP) of the Japanese Data Center for Hematopoietic Cell Transplantation. Patients were included in the study if they had non-M3 AML, were aged 16–65 years, and achieved neutrophil engraftment after their first allogeneic HCT either with single-unit cord blood or a haploidentical-related donor between 2014 and 2020 in Japan. Patients who lacked survival data and GvHD status, and those conditioned with antithymocyte globulin, were excluded.
The primary objective of the study was to understand whether acute GvHD (aGvHD) and chronic GvHD (cGvHD) differs in its impact on overall survival (OS) in CBT recipients and PTCy-haplo-HCT recipients. The secondary objectives included impact of GvHD on leukemia-free survival (LFS), hematologic relapse, and non-relapse mortality (NRM).
Results
The baseline characteristics of patients and transplantations are summarized in Table 1. Compared with the PTCy-haplo-HCT group, the CBT group had significantly more females, a lower complete remission status at HCT, a lower number of HCTs performed between 2018 and 2020, a higher rate of myeloablative conditioning regimens, a higher proportion of GvHD prophylaxis based on calcineurin inhibitors and methotrexate, a higher positive anti-HLA antibody status, and a higher proportion of Grade I–II aGvHD and limited cGvHD (Table 1).
Table 1. Patient, disease, and transplantation characteristics*
|
BM, bone marrow; CBT, cord blood transplantation; CI, calcineurin inhibitor; CMV, cytomegalovirus; CR, complete remission; GvHD, graft-versus-host disease; HCT, hematopoietic cell transplantation; HCT-CI, HCT-specific Comorbidity Index; HLA, human leukocyte antigen; IQR, interquartile range; RIC, reduced-intensity conditioning; ; MMF, mycophenolate mofetil; MTX, methotrexate; PBSC, peripheral blood stem cell. |
|||
|
Characteristic, % (unless otherwise stated) |
Single CBT |
PTCy-haplo-HCT |
p value |
|---|---|---|---|
|
Median age of recipient (IQR), years |
52 (41–60) |
52 (39–59) |
0.248 |
|
Recipient sex |
|
|
0.036 |
|
Female |
48.4 |
41.7 |
|
|
Male |
51.6 |
58.3 |
|
|
Disease status at HCT |
|
|
0.028 |
|
CR |
57.2 |
64.1 |
|
|
Non-CR |
42.8 |
35.9 |
|
|
Year of transplantation |
|
|
<0.001 |
|
2014–2017 |
54.3 |
42.4 |
|
|
2018–2020 |
45.7 |
57.6 |
|
|
Conditioning regimen |
|
|
<0.001 |
|
MAC |
77.1 |
54.5 |
|
|
RIC |
22.9 |
45.5 |
|
|
GvHD prophylaxis |
|
|
<0.001 |
|
CI + MTX |
53.7 |
2.4 |
|
|
CI + MMF |
39.6 |
92.4 |
|
|
Others |
6.7 |
5.2 |
|
|
Graft source |
|
|
<0.001 |
|
BM |
0 |
2.8 |
|
|
PBSC |
0 |
97.2 |
|
|
CB |
100.0 |
0 |
|
|
Number of HLA-A, -B, -DR mismatches |
|
|
<0.001 |
|
0 |
3.8 |
0 |
|
|
1 |
22.9 |
0 |
|
|
2 |
73.3 |
29.7 |
|
|
3 |
0 |
70.3 |
|
|
Anti-HLA antibody |
|
|
0.005 |
|
Negative |
70.2 |
78.5 |
|
|
Positive |
29.8 |
21.5 |
|
|
Acute GvHD by 43 days |
|
|
0.017 |
|
None |
53.4 |
62.1 |
|
|
Grade I–II |
38.3 |
32.4 |
|
|
Grade III–IV |
8.3 |
5.5 |
|
|
Chronic GvHD by 184 days |
|
|
0.039 |
|
None |
78.1 |
83.3 |
|
|
Limited |
13.4 |
8.0 |
|
|
Extensive |
8.5 |
8.7 |
|
Transplantation outcomes
The CBT recipients had significantly higher cumulative incidence of Grade I–II aGvHD at 100 days (48.6% vs 41.0%; p = 0.018), Grade III–IV aGvHD at 100 days (13.0% vs 6.9%; p = 0.001), limited cGvHD at 2 years (17.7% vs 13.2%; p = 0.043), and NRM at 3 years (21.6% vs 14.7%; p = 0.005) compared with PTCy-haplo-HCT recipients. In contrast, the cumulative incidence of relapse was significantly higher in PTCy-haplo-HCT recipients (27.8% vs 20.7% at 3 years; p = 0.005) versus CBT recipients.
Effect of acute and chronic GvHD on post-transplantation outcomes
In univariate analysis, the probability of OS was significantly greater in patients who developed Grade I–II aGvHD and limited cGvHD among CBT recipients, but these effects were not significant among PTCy-haplo-HCT recipients (Figure 1).
In the multivariate analysis, taking no aGvHD as a reference, the reduced effect of Grade I–II aGvHD on overall mortality was significant for CBT (adjusted hazard ratio, 0.73; 95% confidence interval, 0.60–0.87) versus PTCy-haplo-HCT (adjusted hazard ratio, 1.07; 95% confidence interval, 0.70–1.64; p for interaction = 0.038). Whereas, when taking no cGvHD as reference, CBT and PTCy-haplo-HCT had no significant differences on effects of limited and extensive cGvHD on overall mortality.
Figure 1. Univariate analysis of effect of GvHD* on overall survival†
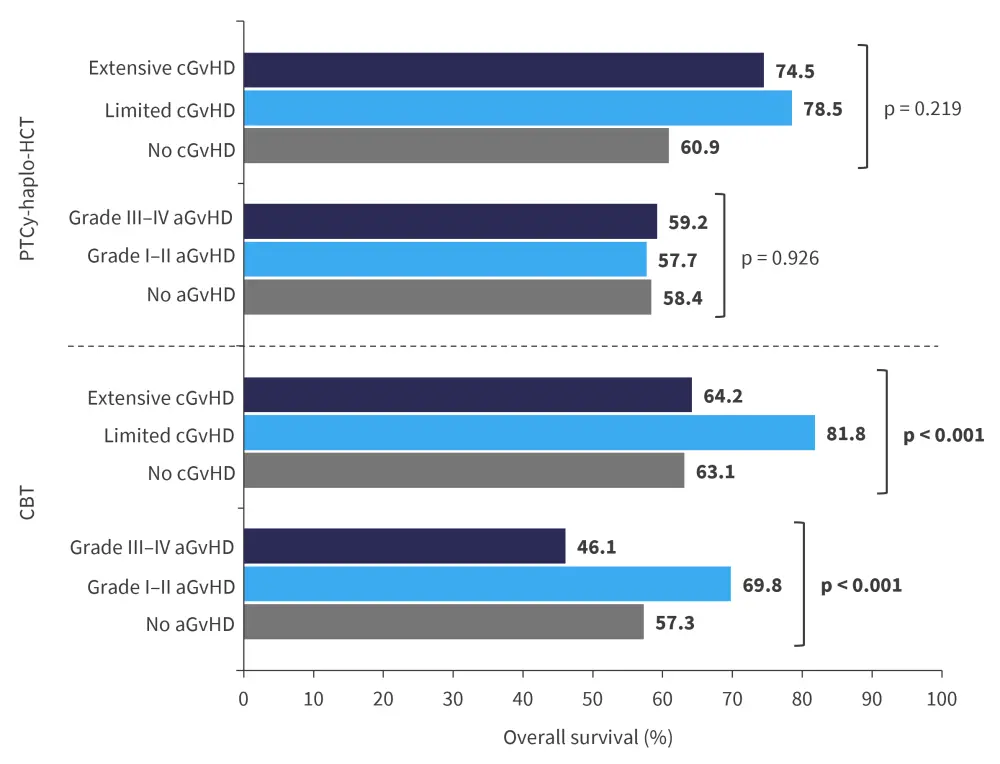
aGvHD, acute GvHD; CBT, cord blood transplantation; cGvHD, chronic GvHD; GvHD, graft-versus-host disease; haplo-HCT, haploidentical hematopoietic cell transplantation; PTCy, post-transplantation cyclophosphamide.
*The landmark day was set at 43 days and 184 days post-HCT, corresponding to when 75% of patients had developed aGvHD and cGvHD, respectively.
†Adapted from Konuma, et al.1
The secondary outcomes are summarized in Figure 2. In the univariate analysis, the probabilities of LFS and cumulative incidence of NRM were greater in patients with aGvHD or cGvHD receiving CBT versus those receiving PTCy-haplo-HCT. Whereas the effects of aGvHD and cGvHD on relapse were non-significant in both the recipient groups (Figure 2).
In the multivariate analysis, the effect of aGvHD and cGvHD on LFS, relapse, and NRM were non-significant in both the recipient groups.
Figure 2. Univariate analysis on effect of GvHD* on A LFS, B relapse, and C NRM†
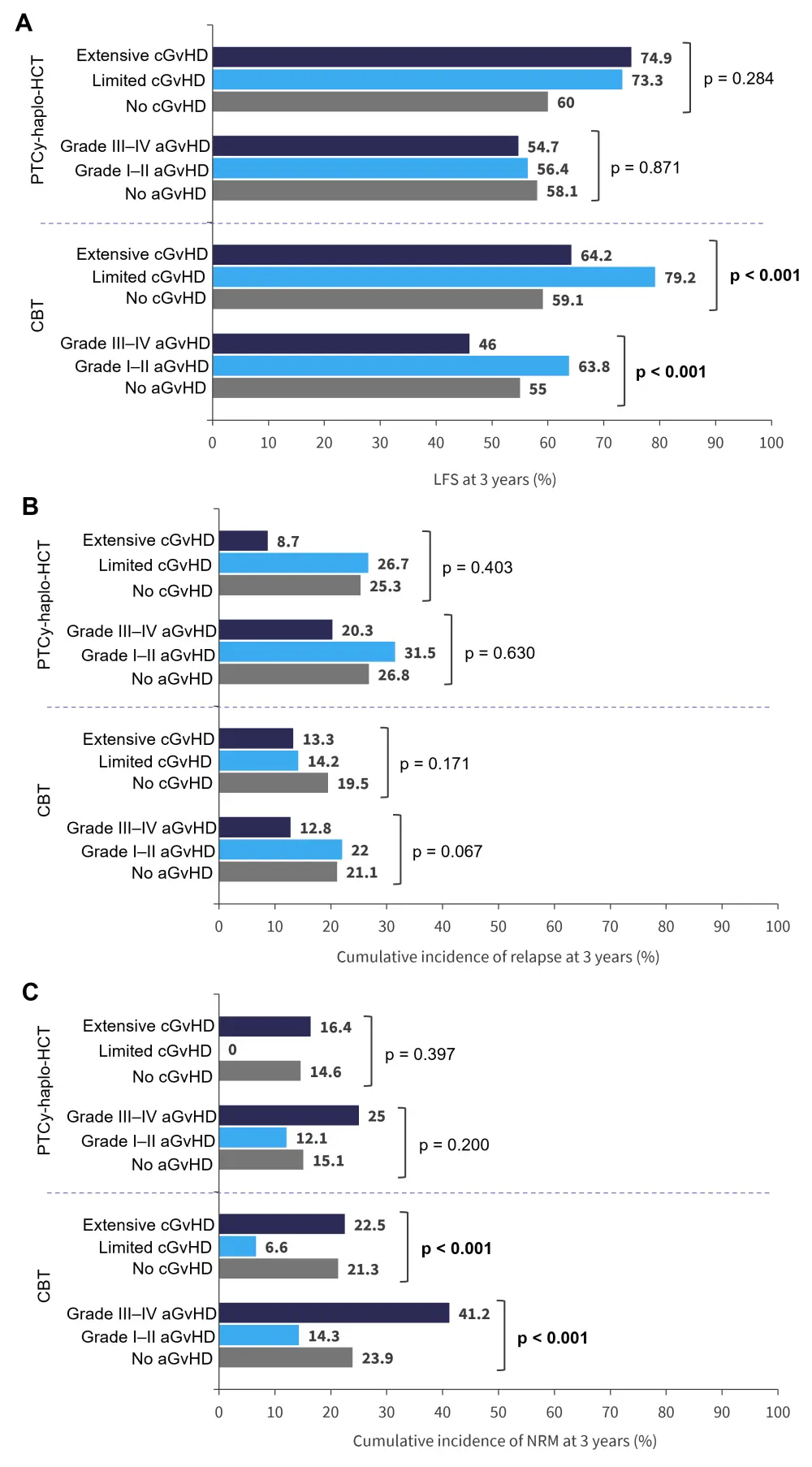
aGvHD, acute GvHD; CBT, cord blood transplantation; cGvHD, chronic GvHD; GvHD, graft-versus-host disease; haplo-HCT, haploidentical hematopoietic cell transplantation; LFS, leukemia-free survival; NRM, non-relapse mortality; PTCy, post-transplantation cyclophosphamide.
*The landmark day was set at 43 days and 184 days post-HCT, corresponding to when 75% of patients had developed aGvHD and cGvHD, respectively
†Adapted from Konuma, et al.1
Conclusion
The authors concluded that the study results suggest mild aGvHD may enhance survival in adult patients with AML receiving CBT, but this was not seen in patients receiving PTCy-haplo-HCT.
The study had few limitations, including selection bias owing to the retrospective nature of the registry-based study, and lack of information on AML genetic profile, HLA-DPB1 mismatch, comparable minimal residual disease status during complete remission, and post-transplantation maintenance therapy, which could have affected the outcomes.
Further research is warranted to clarify the precise mechanism underlying the differential effects between CBT and PTCy-haplo-HCT, and the potential confounding effects of the genetic profile of AML.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?


