All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
Impact of graft CD4/CD8 ratio on HSCT outcomes with different GvHD-prophylaxis regimens
A high CD4/CD8 T-cell ratio in the hematopoietic stem cell transplant (HSCT) allograft is associated with increased risk of graft-versus-host disease (GvHD) and mortality. An optimal GvHD prophylaxis regimen may mitigate this risk; however, the impact of the CD4/CD8 ratio in the graft has not yet been systematically compared using different GvHD prophylaxis regimens.1
To address this knowledge gap, Nikoloudis et al. 1 aimed to analyze the risks associated with a high (i.e., above 75th percentile) CD4/CD8 ratio in HSCT allografts in three different cohorts within a single center, stratified by the applied GvHD prophylactic platforms. Here, we summarize the key findings.
Methods1
This retrospective monocentric study from an Austrian EBMT center included all consecutive HSCTs performed with peripheral blood stem cells between January 21, 2000, and June 29, 2021. The impact of the graft CD4/CD8 ratio was analyzed in the following three cohorts defined by GvHD prophylaxis:
- Cyclosporine A with methotrexate (CSA/MTX; n = 185);
- CSA with mycophenolate mofetil (CSA/MMF; n = 294); and
- Posttransplant cyclophosphamide combined with tacrolimus and MMF (PTCy/TAC/MMF; n = 113).
The impact of the CD4/CD8 ratio was analyzed for endpoints including overall survival (OS), incidence of non-relapse mortality, acute GvHD (aGvHD), chronic GvHD (cGvHD), aGvHD-associated mortality, relapse incidence, and progression-free survival.
Results1
The cohort was stratified according to GvHD prophylaxis regimen. Compared to the CSA/MMF and PTCy-TAC/MMF cohorts, recipients in the CSA/MTX cohort were younger and a higher proportion of patients had a diagnosis of AML or ALL, matched-related donors, and myeloablative conditioning regimens. The key patient and transplant characteristics are summarized in Table 1.
Table 1. Patient characteristics*
|
ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; ATG, antithymocyte globulin; CSA, cyclosporine; MAC, myeloablative conditioning; MDS, myelodysplastic syndrome; MMF, mycophenolate-mofetil; MTX, methotrexate; PTCy, posttransplant cyclophosphamide; RIC, reduced-intensity conditioning; TAC, tacrolimus. |
||||
|
Characteristic, % |
CSA/MMF |
CSA/MTX |
PTCy-TAC/MMF |
p value |
|---|---|---|---|---|
|
Median age of recipient (range), years |
53.68 |
43.96 |
56.96 |
<0.001 |
|
Median age of donor (range), years |
38.40 |
37.16 |
36.90 |
0.77 |
|
Diagnosis |
||||
|
MDS |
25.9 |
15.7 |
22.1 |
0.03 |
|
AML |
40.1 |
54.6 |
46.9 |
|
|
Lymphoma |
20.1 |
10.8 |
17.7 |
|
|
ALL |
12.9 |
16.2 |
11.5 |
|
|
Nonmalignant, |
1.0 |
2.7 |
1.8 |
|
|
Donor type |
||||
|
Matched related |
44.2 |
53.5 |
0 |
<0.01 |
|
Unrelated |
55.8 |
46.5 |
8.8 |
|
|
Haploidentical |
0 |
0 |
91.2 |
|
|
Conditioning |
||||
|
MAC |
43.5 |
80 |
63.7 |
<0.001 |
|
RIC |
56.5 |
20 |
36.3 |
|
|
ATG |
||||
|
No |
23.1 |
40.5 |
— |
<0.001 |
|
Yes |
76.9 |
59.5 |
— |
|
|
Median CD4/CD8 ratio (range) |
1.88 |
1.90 |
1.88 |
0.91 |
|
Median CD3 cell dose (range), 107/kg |
25.54 |
24.80 |
32.47 |
<0.001 |
In the CSA/MMF cohort, a high CD4/CD8 ratio was associated with significantly decreased OS, increased non-relapse mortality, and GvHD-associated mortality (Figure 1). In the PTCy/TAC/MMF cohort, a high CD4/CD8 ratio was associated with significantly lower OS and Grade 3–4 aGvHD. By contrast, a high CD4/CD8 ratio had no significant impact on any of the investigated endpoints in the CSA/MTX cohort (Figure 1).1
Figure 1. Multivariate analyses for study endpoints*
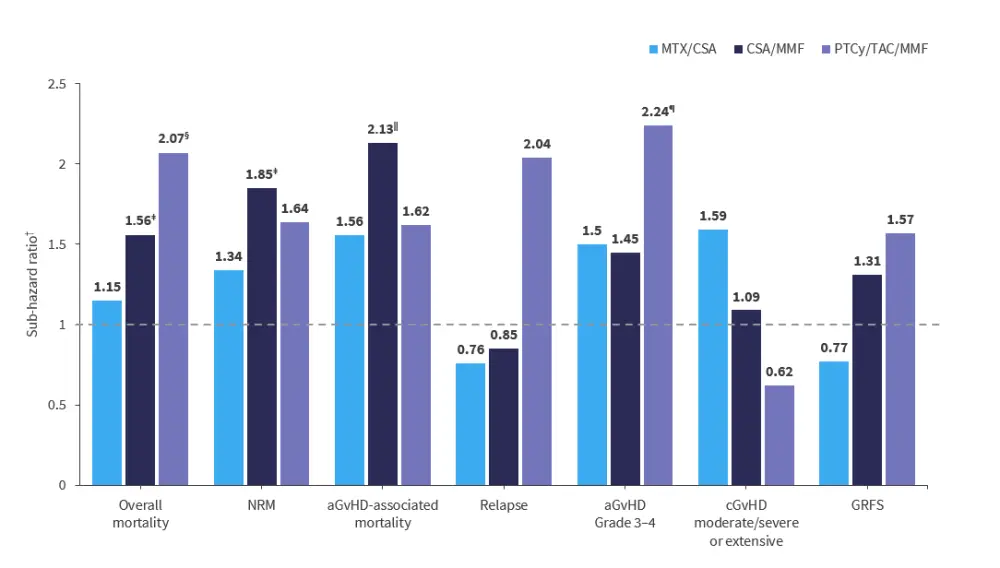
aGvHD, acute GvHD; cGvHD, chronic GvHD; CSA, cyclosporine; GRFS, GVHD and relapse-free survival; GvHD, graft-versus-host disease; MMF, mycophenolate mofetil; MTX, methotrexate; NRM, non-relapse mortality; PTCy, post-transplant cyclophosphamide; TAC, tacrolimus.
*Adapted from Nikoloudis, et al.1
†Sub-hazard ratio > 1 indicates increased probability of an event with high CD4/CD8 ratio compared with low CD4/CD8 ratio.
‡p = 0.01.
§p = 0.04.
ǁp = 0.005.
¶p = 0.02.
In recipients of a HLA-matched transplant who had a top-quartile CD4/CD8 ratio with either an MTX or MMF prophylaxis regimen (n = 116), MTX-based prophylaxis was associated with better OS versus MMF-based prophylaxis. In contrast, in recipients with a lower CD4/CD8 ratio (quartiles 1–3; n = 363), outcomes were identical with MTX versus MMF (Figure 2).
Figure 2. OS in CD4/CD8 ratio subgroups by type of GvHD prophylaxis*
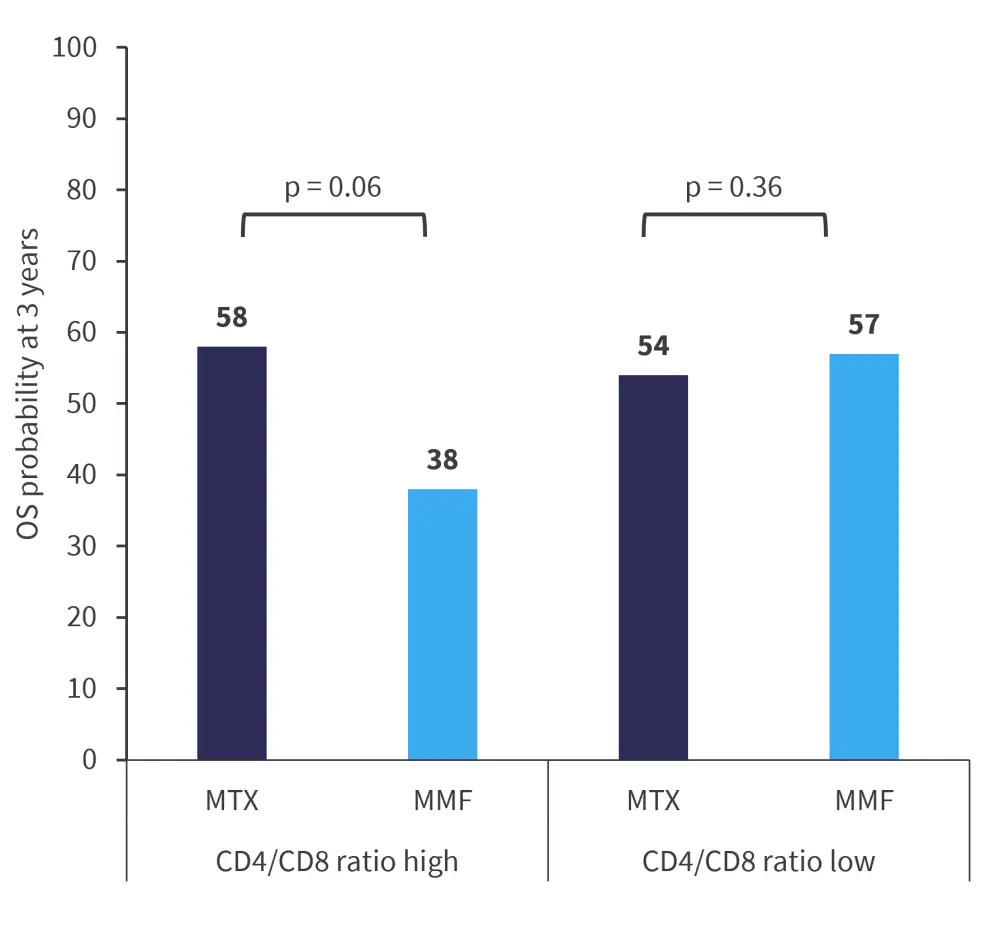
GvHD, graft-versus-host disease; HSCT, hematopoietic stem cell transplant; MMF, mycophenolate-mofetil; MTX, methotrexate; OS, overall survival.
*Adapted from Nikoloudis et al.1
No differences were observed in the impact of high CD4/CD8 ratio on OS when the entire cohort was stratified by median age, conditioning regimen, or median CD3 cell dose. Also, the adverse effect of a high CD4/CD8 ratio was independent of the use of anti-T-lymphocyte globulin and vice versa.
Conclusion1
This study revealed that a high CD4/CD8 ratio in the graft can adversely impact HSCT outcomes, particularly in recipients with post-grafting CSA/MMF and PTCy/TAC/MMF, while MTX-based prophylaxis may largely alleviate this risk factor. Clinical implementation of these results could mean the addition of a short course of MTX (e.g., Day +1 and Day +3) instead of, or in addition to MMF in recipients of grafts with a high CD4/CD8 ratio. Further prospective studies are warranted to better understand the optimal prophylaxis platform for reduced intensity conditioning-based HLA-identical transplants.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?

