All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
Preventative treatment for GvHD in patients requiring haploidentical peripheral blood stem cell transplant: Preliminary findings from the phase II ANZHIT-1 study
In patients who need a stem cell transplant but do not have a human leukocyte antigen (HLA) matched related or unrelated donor, a haploidentical donor transplantation can be considered. Complications such as graft-versus-host disease (GvHD) due to haploidentical hematopoietic stem cell transplant (haplo-HSCT), have recently been overcome with the successful use of posttransplant cyclophosphamide (PTCy), making it increasingly popular. However, hitherto studies of haplo-HSCT using PTCy have been retrospective with multiple different regimes and cell sources, limiting the interpretation of data.
During the 62nd American Society of Hematology (ASH) Annual Meeting and Exposition, John Moore, St Vincent’s Hospital Sydney, AU, presented the preliminary results of a prospective multicenter cohort study (ANZHIT-1; ACTRN12617000151336) that assessed the use of PTCy in patients who had received a predefined conditioning regimen and were undergoing haplo-HSCT 1.
Study design
- A phase II, prospective multicenter cohort study conducted in six Australian centers, stratified 78 patients into two conditioning regimens: reduced intensity conditioning (RIC; n = 46), and myeloablative regimen (MAC; n = 32). See details in Figure 1
- The primary endpoints were disease-free and overall survival at 1 year, while the secondary endpoints were engraftment, cumulative incidence of relapse, transplant-related mortality (TRM), and rates of chronic and acute GvHD
- Patients with a hematopoietic cell transplantation comorbidity index (HCT-CI) > 3 or age > 50 were advised to be on the RIC regimen
Figure 1. RIC and MAC regimens1
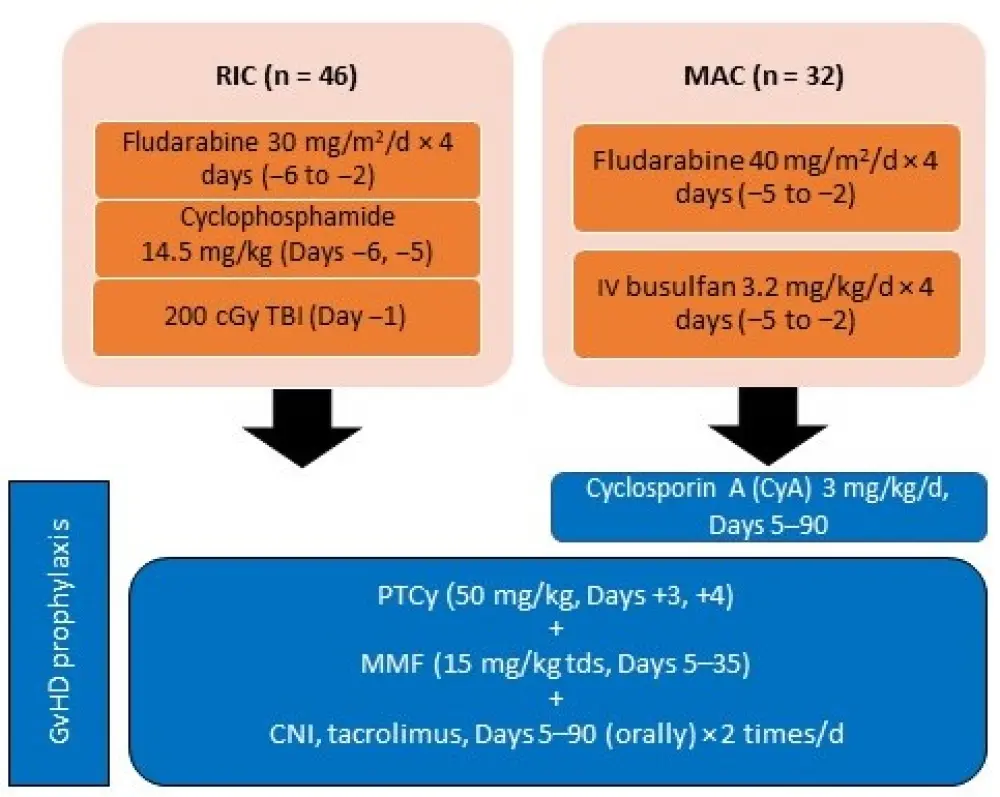
CNI, calcineurin inhibitor; d, day; GvHD, graft-versus-host disease; MAC, myeloablative conditioning; MMF, mycophenolate mofetil; PTCy, posttransplant cyclophosphamide; RIC, reduced intensity conditioning; TBI, total body irradiation; TDS, thrice daily.
Results
Patient baseline characteristics
- A total of 78 patients were included in the study with a median follow-up of 404.5 days (28–1,259)
- Patients receiving MAC were younger and more likely to have ALL as diagnosis. See Table 1 for further details
Table 1. Patient baseline characteristics1
|
ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; DRI, disease risk index; HCT-CI, hematopoietic cell transplantation comorbidity index; HL, Hodgkin lymphoma; MAC, myeloablative conditioning; MDS, myelodysplastic syndromes; NHL, non-Hodgkin lymphoma; RIC, reduced intensity conditioning. |
||
|
Characteristic |
MAC (n = 32) |
RIC (n = 46) |
|---|---|---|
|
Age, Median, years (range) |
38 (18–56) |
59 (20–69) |
|
Age, > 50 MAC, < 50 RIC, n |
6 (all were HCT 1–2) |
6 (4 HL) |
|
HCT-CI, n (range) |
1 (0–1) |
1 (0–5) |
|
High DRI, n |
3 |
7 |
|
Intermediate DRI, n |
18 |
23 |
|
Disease |
||
|
AML, n (%) |
14 (43.7) |
25 (54.3) |
|
ALL, n (%) |
9 (28.1) |
3 (6.5) |
|
MDS, n (%) |
2 (6.25) |
2 (4.3) |
|
NHL, n (%) |
3 (9.3) |
7 (15.2) |
|
HL, n (%) |
0 (0) |
4 (8.7) |
|
Other, n (%) |
5 (15.6) |
5 (10.9) |
Efficacy
- The overall survival rate at 1 year was similar between MAC and RIC patients (74.1% versus 77.8%). See Table 2 for further details.
Safety
- Acute GvHD Grade II–IV rates were high in the RIC arm, while only one patient in the MAC group developed acute Grade III–IV GvHD. Chronic GvHD at 1 year occurred in a high proportion of patients in both groups; however, most were mild to moderate
- TRM at 100 days was low in both groups, showing good tolerability of both regimens. TRM at 1 year increased to 18.8% in MAC patients while it was only 8.7% in RIC patients. Causes for TRM included infection (n = 5), GvHD (n = 3), and veno-occlusive disease (VOD), respiratory failure, and multi-organ failure in one patient each. One case of VOD in the MAC arm was fatal
- Relapse was the most common cause of mortality in RIC treated patients compared with MAC treated patients
Table 2. Primary and secondary outcomes1
|
DFS, disease-free survival; OS, overall survival; GvDH, graft-versus-host disease; MAC, myeloablative conditioning; RIC, reduced intensity conditioning; TRM, transplant-related mortality. |
||
|
Outcome |
MAC (n = 32) |
RIC (n = 46) |
|---|---|---|
|
Follow-up, median (range) |
369 (28–397) |
440 (39–1,259) |
|
Primary OS at 1 year, % (95% CI) |
74.1 (52.9–86.8) |
77.8 (61.6–87.8) |
|
Secondary |
||
|
Neutrophil engraftment, median (range) |
19 (13–92) |
18 (16–40) |
|
Platelet engraftment, median (range) |
30 (13–92) |
38 (24–98) |
|
Relapse rate, % |
6.3 |
17.4 |
|
TRM Day 100, % |
6.3 |
2.2 |
|
TRM 1 year, % |
18.8 |
8.7 |
|
Acute II–IV GvHD, % |
21.9 |
43.5 |
|
Acute III–IV GvHD, % |
3.1 |
21.7 |
|
Chronic GvHD 1 year, % |
31.2 |
43.5 |
|
Severe chronic GvHD (NIH), % |
6.3 |
6.5 |
Conclusion
The study shows encouraging overall survival rates in patients at 1 year irrespective of conditioning regimen. However, early relapse in RIC patients is a concern, while TRM and toxicity profile were significantly higher in patients who received MAC. GvHD rates in both groups are high but majority are mild to moderate acute or chronic GvHD. While relapse seemed to be very well controlled in the MAC arm, a longer follow-up is required to assess relapse rates in both groups. The authors perceived a need for further refinement of the conditioning and GvHD prophylaxis regimen, which they have incorporated in their follow-up phase II multicenter (Australia and New Zealand) ANZHIT-2 study.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?

