All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
Healthcare inequalities in bone marrow transplants
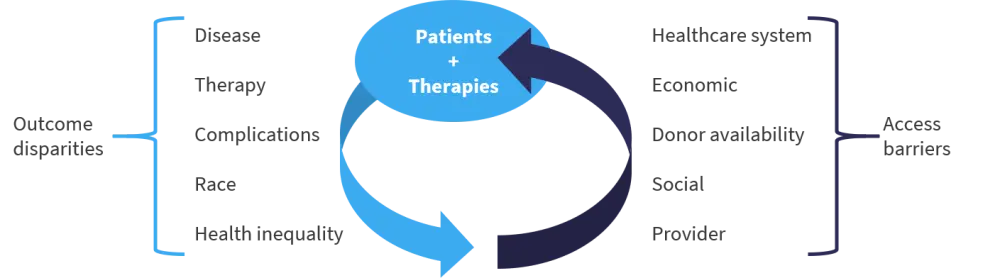
Examining different treatment and diagnostic options for patients undergoing bone marrow transplant (BMT) is an important part of improving outcomes. However, the wider context in which these transplants is occurring is also a crucial part of the equation and can exert great influence on the outcome of therapy. The race and ethnicity of patients can impact how likely a patient is to receive a BMT. The reasons for this are multifactorial and complex, covering a range of issues, including poverty, provider bias, healthcare infrastructure, and social factors (Figure 1).1
Figure 1. Factors affecting access to transplantation*

BMT, bone marrow transplant; HCT, hematopoietic cell transplantation.
*Data from Devine1 and Majhail et al.2
Impact of race and ethnicity on outcomes of therapy
In an article by Ivy Abraham3 published in Blood, patients with acute myeloid leukemia (N = 822) were shown to have different mortality rates dependent on their ethnic backgrounds, with non-Hispanic Black patients faring worse compared with non-Hispanic White patients (hazard ratio, 1.59; 95% confidence interval, 1.15−2.22). This study used data on the level of segregation, wealth, and situation within a particular area or ‘tract’ as identified in a U.S. census as an assessment of structural racism. Out of six composite variables, structural racism was found to be the key factor that accounted for the disparity between outcomes in different ethnic groups.
Bone marrow transplant access
During the Friday Satellite Symposia session on healthcare disparities at the 63rd American Society of Hematology (ASH) Annual Meeting & Exposition, Steven Devine1 discussed some of the issues related to finding bone marrow donor matches that he experiences as the Chief Medical Officer for the National Marrow Donor Program (NMDP), and a summary of these points are shown in Figure 2.
Figure 2. Access barriers and outcome disparities*
*Adapted from Devine.1
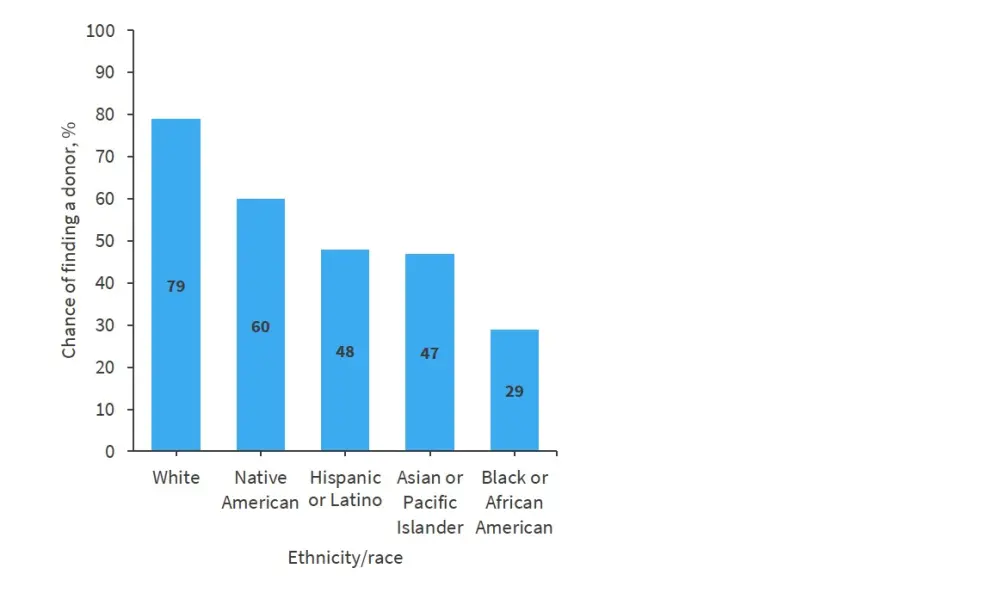
People with the same ethnic background have the best chance of being a match for a patient. In the NMDP, the chance of finding a match for a BMT varies depending on ethnic background. The chance of finding a donor for different ethnicities and race is shown in Figure 3.
Figure 3. Percentage probability of finding a donor for a certain availability*
*Data from Devine.1
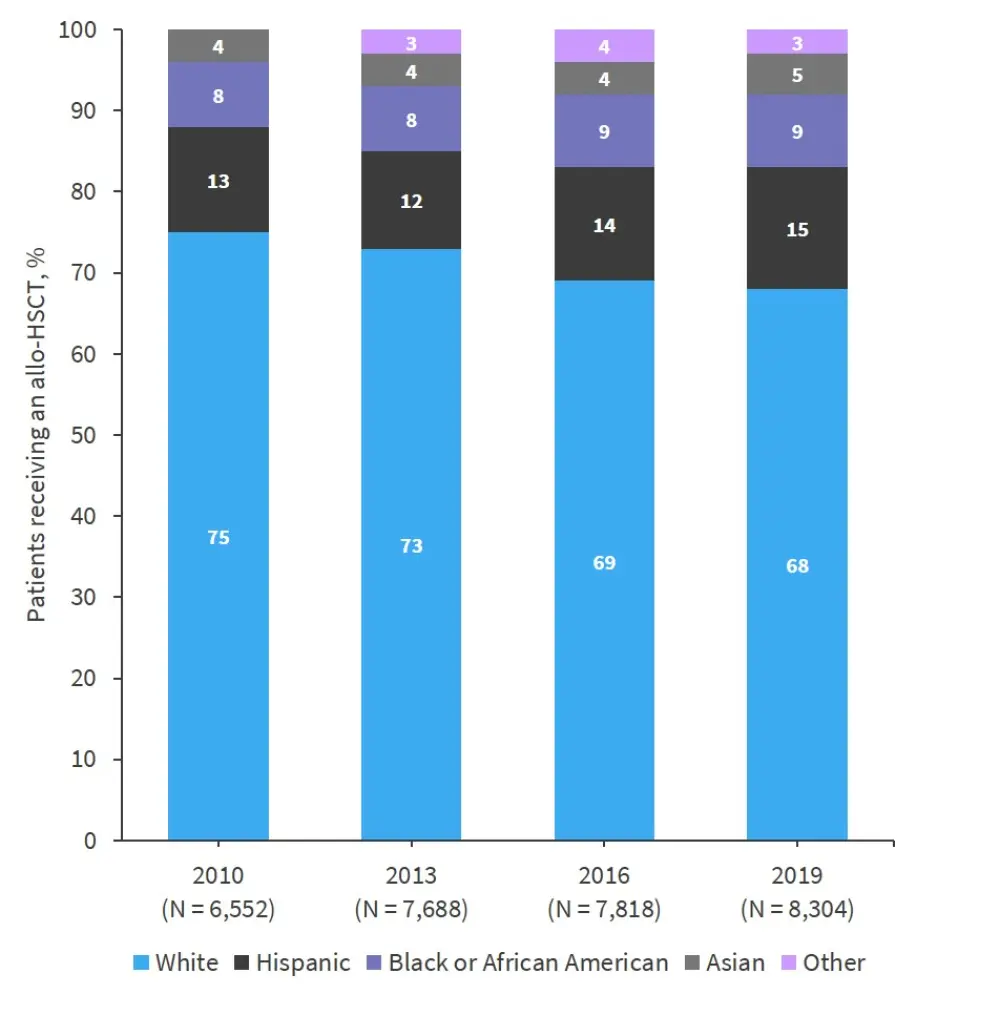
Since 2010, the number of patients receiving an allogeneic hematopoietic stem cell transplant (HSCT) has increased, but the proportion of patients from different ethnic groups has remained similar (Figure 4).
Figure 4. Allo-HSCT trends from 2010 to 2019*
Allo-HSCT, allogeneic hematopoietic stem cell transplant.
*Adapted from Devine.1
Donor availability
In addition to the unequal numbers of donors of different backgrounds on the register, access to transplants is also impacted by donor availability. That is whether a patient on the register when called to donate will be able to give a bone marrow donation. The number of donors on the register is further impacted by availability, resulting in a reduced overall availability of transplant donors across all categories.
Potential solutions
During the session, speakers discussed potential solutions to these problems.
Donor pool expansion
Steven Devine1 discussed ways to overcome the problems with poor donor availability in certain ethnic groups. He performed a thought experiment to add 11 million African Americans (AFA) to the register and, assuming 100% availability, showed an increase in match rates to 63.7%, which could greatly increase the number of lives saved. Although such a large instantaneous addition is not possible, increasing the number of donors from key ethnic groups, such as AFA and Hispanic populations, is a key goal for the NMDP.
The NMDP aim to do this by seeking to improve education about their work. The donor registry for AFA is skewing towards younger donors, with a median age of 24 years when signing up, which is very positive. Visiting schools to tell children about these programs prior to them being able to sign up for them is one method of getting the message out, along with other community outreach campaigns.
Another approach is to try to improve cooperation and ease of access between international registries. For example, sharing data with Brazil could improve access to donors for Hispanic patients in a more cost-effective manner than recruiting a comparable number in the U.S. where the NMDP is based.
The number of matched donors available also depends on the stringency of matching criteria. If a match is required to be an 8/8 human leukocyte antigen (HLA) match, the number of donors required is much greater than if 7/8 HLA matches or below are tolerated. For AFA, allowing 7/8 or 6/8 HLA matches would increase the percentage match rate to 72% or 97%, respectively.
Alternative donors
Nicholas Kroeger4 expanded on the idea of using alternative donor types for BMT. Matched sibling donors are only available for 30% of patients. As discussed previously, matched unrelated donors can be found for a high proportion of non-Hispanic white patients, but a low percentage of AFA patients.
Kroeger highlighted the BMT CTN 1101 trial (NCT01597778), which compared haplo-identical BMT with double unrelated umbilical cord blood (UCB) transplantation. In this trial, patients who had received transplants from haploidentical donors showed improved overall survival (OS) and graft-versus-host disease (GvHD)-free relapse-free survival compared with those who received an UCB transplantation. Haploidentical transplants have the advantage that most patients should have at least one haploidentical donor (parents or children) accessible. However, HLA mismatches trigger a robust T-cell mediated graft-versus-host response, which can result in poor long-term outcomes.
- To overcome this, two alternative approaches have been studied: the use of alloreactive donor T-cell depleted transplants, and unmanipulated haplo-BMT given with anti-thymocyte globulin, post-transplant cyclophosphamide (PTCy), or using granulocyte-colony stimulating factor primed grafts
Kroeger concluded that current studies favor the use of PTCy with haploidentical donors over UCB or mismatched unrelated donors.
Reduced incidence and severity of GvHD
Christopher Kanakry5 further discussed the use of PTCy as a method of preventing severe acute GvHD (aGvHD) and chronic GvHD (cGvHD) following haploidentical HSCT. There is a delicate balance between achieving a robust graft-versus-leukemia effect while not triggering unmanageable GvHD. Kanakry showed that PTCy prevention of cGvHD does not appear to result in an increased risk of relapse, with 3-year outcomes of patients treated with reduced intensity conditioning (Table 1).
Table 1. Survival outcomes between patients treated with PTCy haplo-HSCT and MUD HSCT*
|
CIBMTR, Center for International Blood and Marrow Transplant Research; HSCT, hematopoietic stem cell transplant; MRD, measurable residual disease; MUD, matched unrelated donor; OS, overall survival; PFS, progression free survival; PTCy, post-transplant cyclophosphamide; RIC, reduced intensity conditioning. |
||
|
3-year outcomes, % |
RIC haplo-HSCT using PTCy |
RIC MRD and MUD HSCT |
|---|---|---|
|
PFS |
|
|
|
Low-risk |
65 |
66 |
|
High-risk |
25 |
15 |
|
OS |
|
|
|
Low-risk |
73 |
70 |
|
High-risk |
37 |
25 |
In patients with lymphoma, lower rates of cGvHD have been observed with the use of PTCy in haploidentical HSCT compared with HLA-matched sibling HSCT, with similar survival rates between the comparison groups. In addition, Kanakry presented data to show that patients treated with PTCy following HLA-matched peripheral blood HSCT have superior outcomes to those on standard GvHD prophylaxis.
Alternative GvHD prevention strategies
In the final healthcare disparities presentation, Muna Qayed6 spoke about GvHD prophylaxis outside of PTCy. Abatacept, which prevents T-cell stimulation, has been investigated for preventing aGvHD in the ABA2 study compared with a calcineurin inhibitor and methotrexate. Abatacept reduced the incidence of aGvHD in both matched unrelated donor (MUD)- and mismatched unrelated donor (MMUD)-transplanted patients, and it improved survival in the MMUD cohort compared with MUD historical controls.
PTCy in combination with different agents, such as bortezomib or abatacept, may also increase the ability to use 7/8 HLA-matched donors. PTCy + bortezomib was shown to result in Grade II–IV GvHD in 35% and cGvHD in 34%, with a 1-year treatment-related mortality rate of 14% and a 1-year OS of 72%.
Qayed also discussed sitagliptin, an inhibitor of dipeptidyl peptidase 4, which has a costimulatory function in activating T cells. Sitagliptin has been assessed in a phase II trial with tacrolismus and sirolismus (NCT02683525). This trial produced a 1-year non-relapse mortality rate of 0%, along with a cumulative incidence of cGvHD at 1-year of 37% and an OS at 1-year of 94%.
Conclusion
The session concluded that healthcare disparities in BMT remain a very real problem and overcoming these issues will require a multipronged approach. Encouraging donors from different ethnic backgrounds to join the bone marrow registry is part of the answer, but this will not eliminate the challenge of finding a donor for everyone who needs one. To encourage more AFA and other ethnic groups to donate, fundamental issues within our society require addressing, such as structural racism. This means that we must find alternative solutions to address these ongoing issues.
The use of alternative donor options holds promise, with the ability to use MMUDs that are tolerable to patients, possibly being the key to enabling BMT in many more patients. Both aGvHD and cGvHD remain a formidable problem, but ongoing trials with PTCy and other novel agents are producing interesting results and may help to lessen the racial and ethnic disparities in HSCT outcomes.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?

