All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
In patients who undergo allogeneic hematopoietic stem cell transplantation, a combination of a calcineurin inhibitor plus methotrexate (MTX) is used as the standard regimen for graft-versus-host disease (GvHD) prophylaxis. During the phase III Bone Marrow Transplant Clinical Trials Network (BMT CTN) 1703 study (NCT03959241), the combination of posttransplant cyclophosphamide (PTCy) with tacrolimus (TAC) and mycophenolate mofetil (MMF) demonstrated lower incidences of severe acute GvHD, chronic GvHD, and better GvHD-free relapse-free survival when compared with the TAC/MTX combination for the prevention of GvHD.1,2 However, the control arm did not include antithymocyte globulin (ATG), which is commonly used as a GvHD prophylaxis.
During the 2024 Transplantation & Cellular Therapy Meetings of ASTCT and CIBMTR, Aron Nagler presented real-world data evaluating posttransplant outcomes of PTCy or ATG combined with TAC or cyclosporine A (CsA), and with MMF or MTX for the prevention of GvHD.1 Here, we summarize the key points from the poster below
Study design1
- This was a registry-based retrospective analysis of patients with acute myeloid leukemia who underwent allogeneic hematopoietic stem cell transplantation from matched siblings or 9─10/10 unrelated donors in first complete remission.
- This study compared PTCy with TAC or CsA and MMF with ATG combined with TAC or CsA and MTX for GvHD prophylaxis.
- Posttransplant outcomes were measured using statistical tests including a multivariate analysis which was adjusted for potential confounding factors using a Cox proportional-hazards regression model.
Key findings
- In total, 6,050 patients were included in this retrospective study
- 402 patients received PTCy with CsA or TAC and MMF
- 5,648 patients received ATG with CsA or TAC and MTX
- Patients in the PTCy with CsA or TAC and MMF group were younger, with a median age of 48.7 years, compared with the ATG with CsA or TAC and MTX group, in which patients had a median age of 51.5 years (p = 0.024)
- The median follow-up was 23.4 months in the PTCy with CsA or TAC and MMF group and 41.8 months in the ATG with CsA or TAC and MTX group (p < 0.0001).
- A similar incidence and severity of acute GvHD were observed in both the PTCy with CsA or TAC and MMF, and ATG with CsA or TAC and MTX cohorts (Figure 1).
Figure 1. Occurrence of acute GvHD in patients posttransplant*
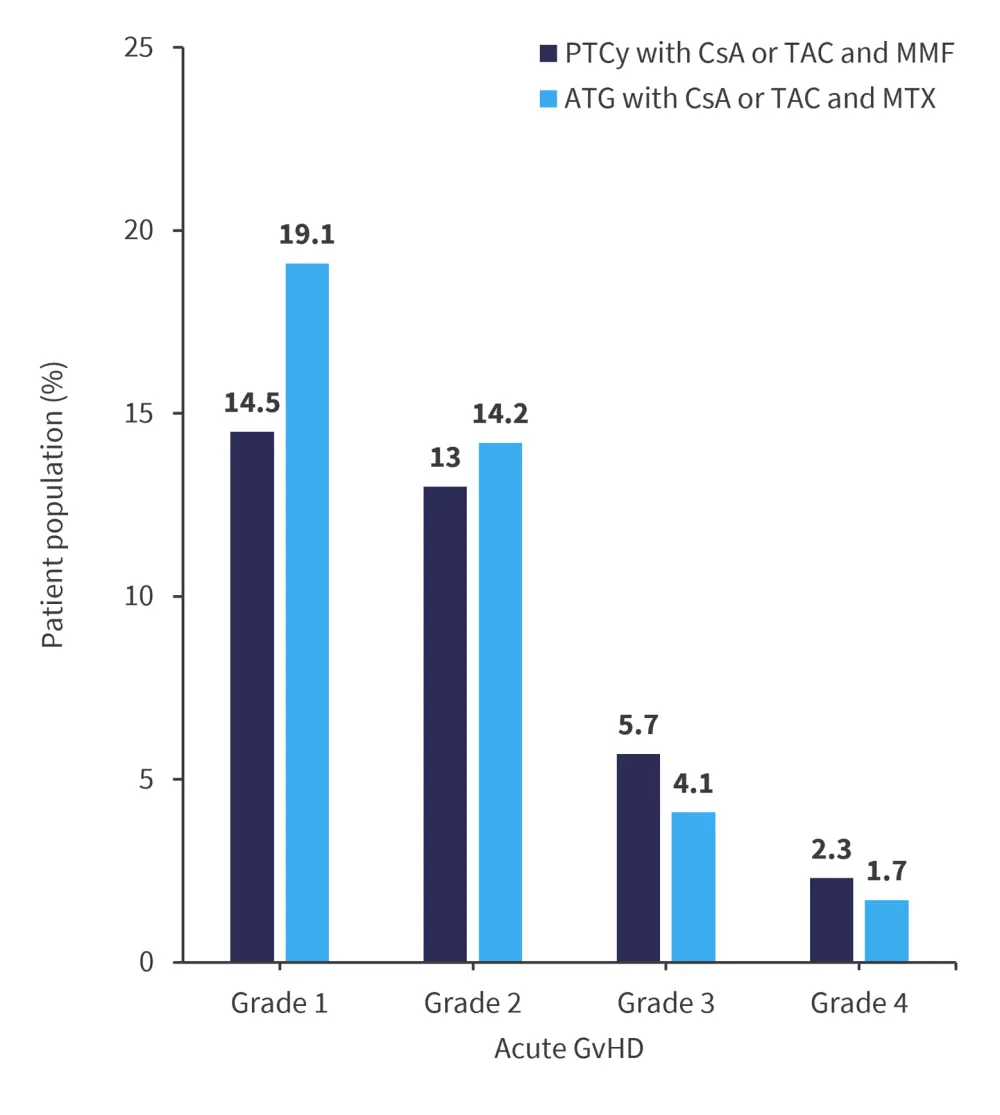
ATG, antithymocyte; CsA, cyclosporin; GvHD, graft-versus-host disease; MMF, mycophenolate mofetil; MTX, methotrexate; PTCy, posttransplant cyclophosphamide; TAC, tacrolimus.
*Data from Nagler.1
- Non-relapse mortality was significantly lower in the PTCy with CsA or TAC and MMF cohort compared with the ATG with CsA or TAC and MTX cohort; all other transplant outcome parameters were similar across both cohorts (Table 1).
- GvHD was the cause of death for a similar number of patients in both the PTCy with CsA or TAC and MMF and the ATG with CsA or TAC and MTX cohorts (11.6% and 13.9%, respectively).
Table 1. Multivariate analysis for posttransplant responses*
|
|
Relapse |
NRM |
OS |
|||
|---|---|---|---|---|---|---|
|
HR |
p-value |
HR |
p-value |
HR |
p-value |
|
|
PTCy with CsA or TAC and MMF vs ATG with CsA or TAC and MTX |
0.99 |
0.93 |
1.57 |
0.022† |
1.18 |
0.16 |
|
ATG, antithymocyte; CI, confidence interval; CsA, cyclosporin; HR, hazard ratio; MMF, mycophenolate mofetil; MTX, methotrexate; NRM, non-relapse mortality; OS, overall survival; PTCy, posttransplant cyclophosphamide; TAC, tacrolimus. |
||||||
|
Key learnings |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?


 Arnon Nagler
Arnon Nagler