All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
Biomarkers and risk factors in flares of aGvHD: MAGIC analysis
Patients who undergo allogeneic hematopoietic cell transplant (allo-HCT) are at risk of developing acute graft-versus-host disease (aGvHD).1 The current standard first-line treatment for aGvHD is systemic steroids.1 However, aGvHD symptoms often flare in patients upon tapering or discontinuation of steroids.1 The lack of data available for incidence, clinical presentations, and outcomes of aGvHD flares, and the absence of a standardized definition for GvHD flares makes it challenging to assess patients at risk of these occurrences.1
Focusing on the use of serum biomarkers, below, we summarize data evaluating flares of aGVHD in the Mount Sinai Acute GvHD International Consortium (MAGIC) analysis, published by Akahoshi et al.1 in Blood Advances.
Study design1
- A retrospective study of adult and pediatric patients who received allo-HCT at 23 international allo-HCT centers in North America, Europe, and Asia, between 2014 and 2021.
- Patients were eligible for this study if they achieved complete response (CR) or very good partial response (VGPR) to systemic steroid treatment, within 4 weeks without primary disease relapse.
- The definition of aGvHD flare was defined according to expert consensus in the Mount Sinai Acute GvHD International Consortium.
- Serum samples were collected at the initial achievement of CR/VGPR.
- The MAGIC algorithm probability was calculated as a value between 0.001 and 0.999.
- Validated thresholds for Ann Arbor (AA) scores were used (AA1 < 0.14; 0.14 ≤ AA2 < 0.29; AA3 ≥ 0.29).
Key findings1
- In total, 968 patients were included in this study.
- The cumulative incidence of flares after CR/VGPR at 6 months was 21.6% (95% confidence interval [CI], 19.0–24.2%).
- Patients with Grade 3–4 GvHD, at the time of flare, were more likely to experience non-relapse mortality than those with Grade 1–2 GvHD (47% vs 12%; p<0.001).
- After measuring the MAGIC algorithm probability score in all patients at CR/VGPR, the cumulative incidence of eventual flares increased with each AA score increase (Figure 1.).
Figure 1. Cumulative incidence of flares measured by MAPs at CR/VGPR*
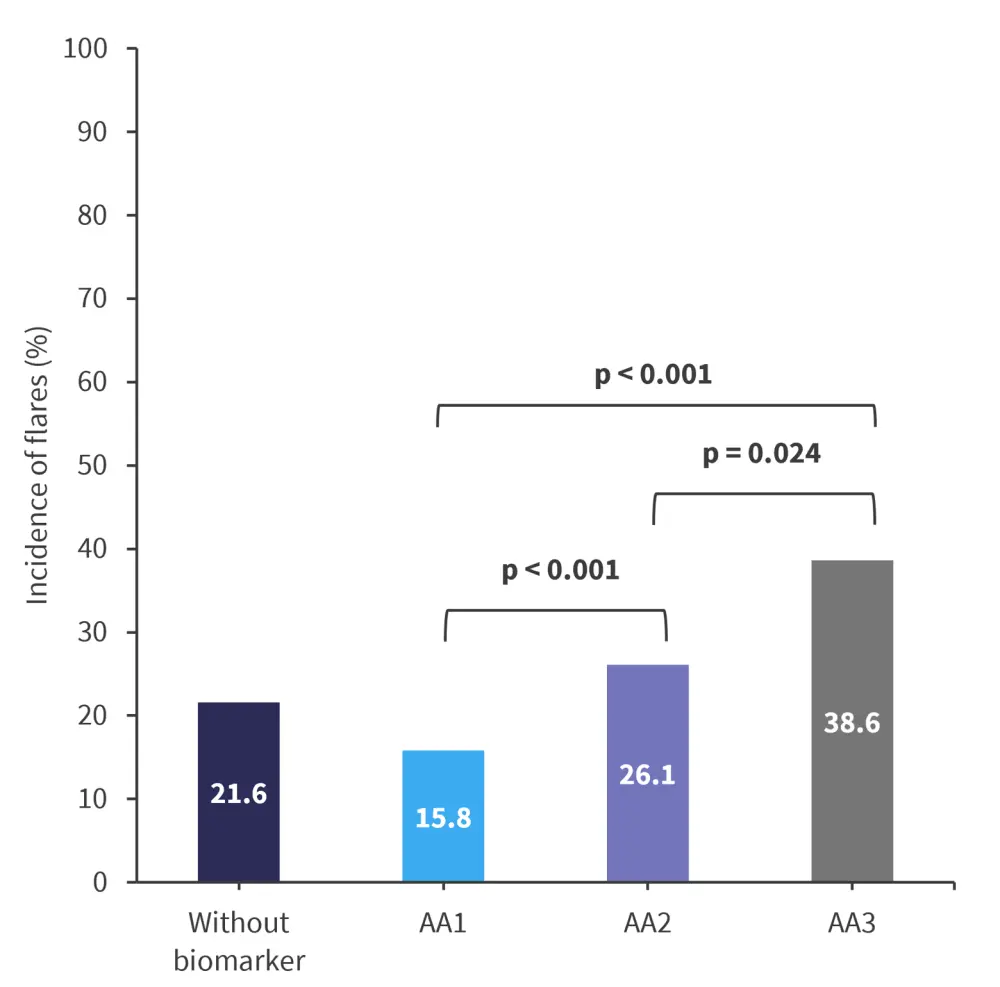
AA, Ann Arbor; CR, complete response; MAP, Mount Sinai Acute GvHD International Consortium algorithm predictor; VGPR, very good partial response.
*Data from Akahoshi, et al.1
- Patients whose steroids were tapered rapidly were nearly twice as likely to experience a flare compared with patients who were tapered slowly (30% vs 17%; p < 0.001).
- In patients who developed Grade 3–4 GvHD, the severity of flare and proportion of patients with lower gastrointestinal involvement (Stage 2–4) increased with each increase of AA score (Table 1).
Table 1. Severity and LGI involvement measured by MAPs at CR/VGPR*
|
AA, Ann Arbor; CR, complete response; GI, gastrointestinal; LGI, lower GI; MAP, Mount Sinai Acute GVHD International Consortium algorithm predictor; VGPR, very good partial response. |
|||
|
|
AA1 |
AA2 |
AA3 |
|---|---|---|---|
|
Severity, % |
5.4 |
11.4 |
20.0 |
|
Lower GI involvement, % |
4.9 |
9.9 |
18.0 |
|
Key learnings1 |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?


