All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
A phase II trial of PTCy versus ATG for GvHD prophylaxis after RIC regimen allo-HCT
The development of graft-versus-host disease (GvHD) can significantly impact the outcomes of patients who have received allogeneic hematopoietic cell transplantation (allo-HCT). Rabbit antithymocyte globulin (ATG) is recommended for GvHD prophylaxis in the matched-unrelated donor allo-HCT setting. Another agent, posttransplant cyclophosphamide (PTCy) is also used successfully for preventing both acute and chronic GvHD in patients undergoing transplantation. However, there is a lack of data comparing the use of these two agents in 10/10 human leukocyte antigen (HLA)-matched donor transplants.
During the 47th Annual Meeting of the European Society for Blood and Marrow Transplantation (EBMT), Eolia Brissot presented the results of a multicenter, randomized, phase II trial (NCT02876679) comparing the efficacy of PTCy versus ATG for GvHD prophylaxis in patients undergoing fludarabine–busulfan reduced-intensity conditioning (RIC) regimen allo-HCT with 10/10 HLA-matched donors.1 The EBMT Board selected this abstract for the Van Bekkum Award, and the GvHD Hub is happy to provide a summary.
Study design
The treatment arms are detailed in Figure 1. All patients had availability of either a matched sibling or 10/10-matched unrelated donor and received a graft source of peripheral blood stem cells.
- Primary endpoint: To determine the efficacy of PTCy (experimental arm) versus ATG (control arm) for GvHD prophylaxis after 12 months, measured by the composite endpoint of GvHD-free, relapse-free survival (GRFS).
- Secondary endpoints:
- Occurrence of acute and chronic GvHD;
- Disease-free survival (DFS) and overall survival (OS);
- Non-relapse mortality (NRM) and relapse incidence; and
- Quality of life.
An immune recovery study helped to increase understanding of the PTCy and ATG mechanisms of action in GvHD.
Figure 1. Treatment schema*
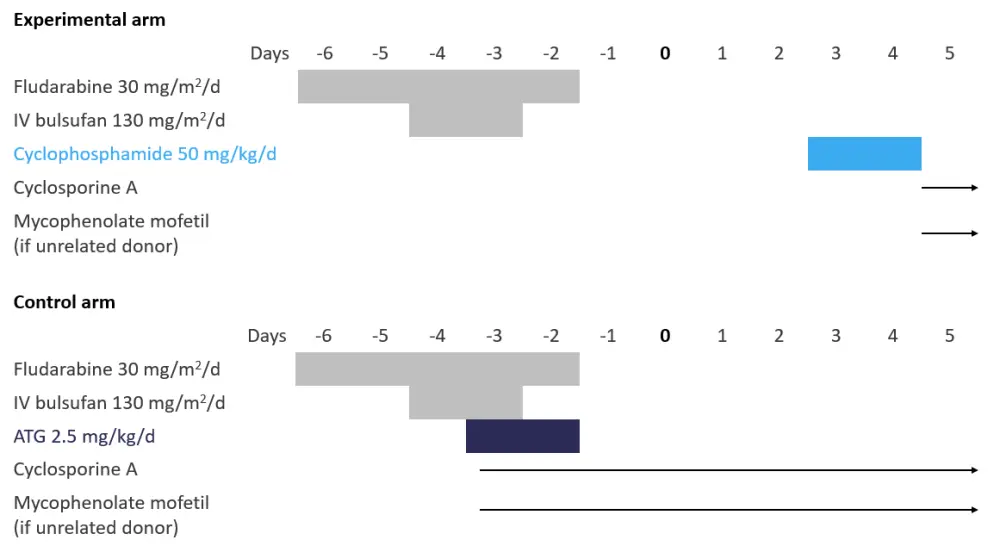
ATG, antithymocyte globulin; d, day; IV, intravenous.
*Adapted from Brissot et al.1
Patient characteristics
In total, 89 patients were randomized in a 1:1 ratio between 2017 and 2019, 80 of which went on to undergo allo-HCT. The demographics for patients and baseline transplant characteristics were well balanced between the two arms. Selected characteristics of patients who underwent transplant during the study are shown in Table 1.
Table 1. Selected patient and transplant characteristics*
|
ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; ATG, antithymocyte globulin; CR1, first complete remission; ECOG, Eastern Cooperative Oncology Group; HL, Hodgkin lymphoma; MDS, myelodysplastic syndromes; MM, multiple myeloma; MSD, matched sibling donor; MUD, matched unrelated donor; NHL, non-Hodgkin lymphoma; PR, partial remission; PTCy, posttransplant cyclophosphamide. |
||
|
|
PTCy arm |
ATG arm |
|---|---|---|
|
Patient characteristics |
||
|
Median age, years (range) |
64.9 (36.0–71.1) |
64.3 (21.3–70.7) |
|
Gender, % |
||
|
Male |
69.8 |
70.3 |
|
Disease, % |
||
|
AML |
48.8 |
45.9 |
|
Status, % |
||
|
At diagnosis |
2.4 |
5.6 |
|
ECOG status, % |
||
|
0 |
59.0 |
57.6 |
|
Transplant characteristics |
||
|
Donor type, % |
||
|
MSD |
37.2 |
40.5 |
Results
The primary endpoint of 1-year GRFS after transplantation was comparable in both the PTCy and ATG groups. No significant distinctions were observed between the two study arms for all secondary endpoints, namely OS, DFS, NRM, Grade II-IV and III-IV acute GvHD, and chronic GvHD. Results for key study outcomes are presented in Table 2.
Table 2. Primary and secondary endpoint results*
|
ATG, antithymocyte globulin; DFS, disease-free survival; GRFS, GvHD-free, relapse-free survival; NRM, non-relapse mortality; OS, overall survival; PTCy, posttransplant cyclophosphamide. |
|||
|
|
PTCy arm |
ATG arm |
p value |
|---|---|---|---|
|
Primary endpoint, % (95% CI) |
|||
|
GRFS |
52.2 (36.0–66.2) |
52.2 (26.1–57.5) |
0.38 |
|
Secondary endpoints, % (95% CI) |
|||
|
Acute GvHD† |
|
|
|
|
Chronic GvHD ‡ |
26.0 (13.8–40.0) |
30.2 (16.1–45.5) |
0.56 |
|
DFS‡ |
68.5 (51.6–80.5) |
67.1 (49.4–79.8) |
0.68 |
|
OS‡ |
78.9 (63.4–88.4) |
80.4 (63.1–90.2) |
0.93 |
|
NRM |
14.0 (5.6–26.1) |
10.8 (10.2–36.8) |
0.75 |
The main adverse events focusing on viral reactivation and cardiac adverse events are presented in Table 3. Similarly, no statistically significant differences were observed between the two groups of the study.
Table 3. Selected adverse events*
|
AE, adverse event; ATG, antithymocyte globulin; CMV, cytomegalovirus; EBV, Epstein–Barr virus; PTCy, posttransplant cyclophosphamide. |
|||
|
AE |
PTCy arm |
ATG arm |
p value |
|---|---|---|---|
|
EBV reactivation, % |
11.6 |
18.9 |
0.36 |
|
CMV reactivation, % |
23.3 |
27 |
0.70 |
|
Cardiac AE, % |
14 |
8.1 |
0.49 |
|
Hemorrhagic cystitis, % |
7 |
2.7 |
0.62 |
Conclusion
These results indicate that the use of PTCy for GvHD prophylaxis resulted in similar outcomes to those seen with ATG for patients who underwent an fludarabine–busulfan RIC regimen allo-HCT with a 10/10 HLA-matched related or unrelated donor. Therefore, both PTCy and ATG can be used for GvHD prophylaxis in this setting.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?

