All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
Validity of the Minnesota aGvHD risk score in predicting survival and response to therapy
The Minnesota acute graft-versus-host disease (aGvHD) risk score was developed to classify patients as standard- or high-risk of non-relapse mortality and response to therapy. The scoring system considers the number of organs involved and the severity of aGvHD at therapy onset, with standard-risk patients showing better outcomes.1
At the 48th Annual Meeting of the European Society for Bone and Marrow Transplantation (EBMT), Maria Teresa Lupo-Stanghellini1 presented a single-center study investigating the efficacy of this scoring system in the setting of posttransplant cyclophosphamide (PTCy). In this article we summarize the key results.
You can listen to a summary of the Minnesota risk score for GvHD in our interview with David Weisdorf here:
How do we stratify risk in patients with GvHD?
Methods
This prospective single-center study aimed to identify the accuracy of the Minnesota risk score in identifying patients at high-risk of aGvHD-associated mortality and response to steroid therapy. Inclusion criteria were:
- allogeneic hematopoietic stem cell transplants performed at San Raffaele Hospital, IT;
- recipients of PTCy-based GvHD prophylaxis for any disease indication;
- any donor type;
- and transplants performed between January 2016 and June 2020.
Results
Out of 315 eligible patients, 139 developed aGvHD, and their characteristics are summarized in Table 1.
Table 1. Characteristics of patients who developed aGvHD*
|
aGvHD, acute graft-versus-host disease; ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; HL, Hodgkin lymphoma; MAC, myeloablative conditioning; MDS, myelodysplastic syndromes; MPN, myeloproliferative neoplasms; NHL, non-Hodgkin lymphoma; RIC, reduced intensity conditioning. |
|
|
Characteristic, % (unless otherwise stated) |
n = 139 |
|---|---|
|
Median follow-up (range), years |
2.4 (1.4–3.5) |
|
Median age (range), years |
52.7 (15.3–75.6) |
|
Sex |
|
|
Male |
62.6 |
|
Female |
37.4 |
|
Diagnosis |
|
|
AML |
50.4 |
|
ALL |
12.2 |
|
NHL/HL |
10.8 |
|
MDS or MPN |
23.7 |
|
Other |
2.9 |
|
Disease risk index |
|
|
Low-intermediate |
55.4 |
|
High |
28.8 |
|
Very high |
5.8 |
|
Donor |
|
|
Mismatched related donor |
48.2 |
|
Matched related donor |
12.9 |
|
Matched unrelated donor |
38.9 |
|
Conditioning |
|
|
MAC |
70.5 |
|
RIC |
28.8 |
|
Graft source |
|
|
Bone marrow |
5.8 |
|
Peripheral blood |
94.2 |
|
Minnesota risk |
|
|
High-risk |
33.1 |
|
Standard-risk |
66.9 |
Multivariate analysis of all patients indicated that:
- the development of both Grades II–IV and III–IV aGvHD were impacted by donor source and donor age, with older donors associated with worse disease (Table 2);
- and the development of aGvHD Grade III–IV was affected by donor source (Table 2).
Table 2. Multivariate analysis of factors associated with aGvHD incidence*
|
aGvHD, acute graft-versus-host disease; CI, confidence interval; HR, hazard ratio; MMRD, mismatched related donor; MRD, matched related donor; MUD, matched unrelated donor. |
||||
|
Characteristic |
aGvHD Grade II–IV |
aGvHD Grade III–IV |
||
|---|---|---|---|---|
|
HR (95% CI) |
p value |
HR (95% CI) |
p value |
|
|
Donor source |
|
0.01 |
|
0.003 |
|
MRD vs MMRD |
0.27 (0.13–0.57) |
0.001 |
0.163 (0.05–0.55) |
0.003 |
|
MUD vs MMRD |
0.54 (0.30–0.99) |
0.047 |
0.45 (0.21–0.96) |
0.039 |
|
Donor age |
|
|
|
|
|
>35 years vs ≤35 years |
2.75 (1.59–4.76) |
<0.001 |
— |
— |
Rates of 2-year overall survival and transplant-related mortality (TRM) stratified by Minnesota risk score revealed improved survival and lower TRM in patients with a standard risk score compared with those classified as high-risk (Figure 1).
Figure 1. The 2-year OS and TRM in Minnesota high- and standard-risk patients*
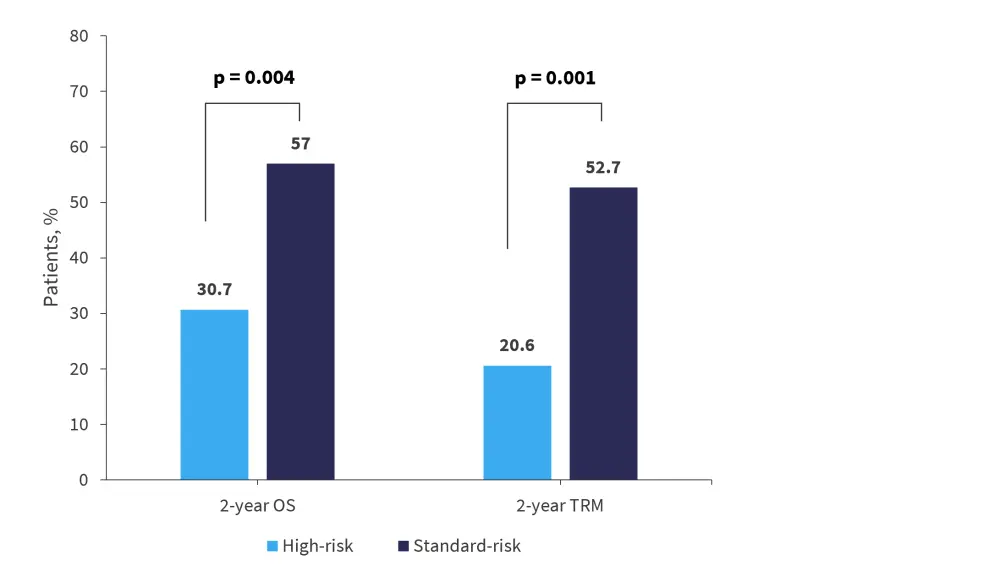
OS, overall survival; TRM, transplant-related mortality.
*Adapted from Lupo-Stanghellini.1
When stratifying by Day 28 overall response rate, improved response rates were seen in the standard-risk cohort compared with the high-risk cohort (Figure 2).
Figure 2. Day 28 ORR in patients classified as standard- and high-risk by Minnesota score*
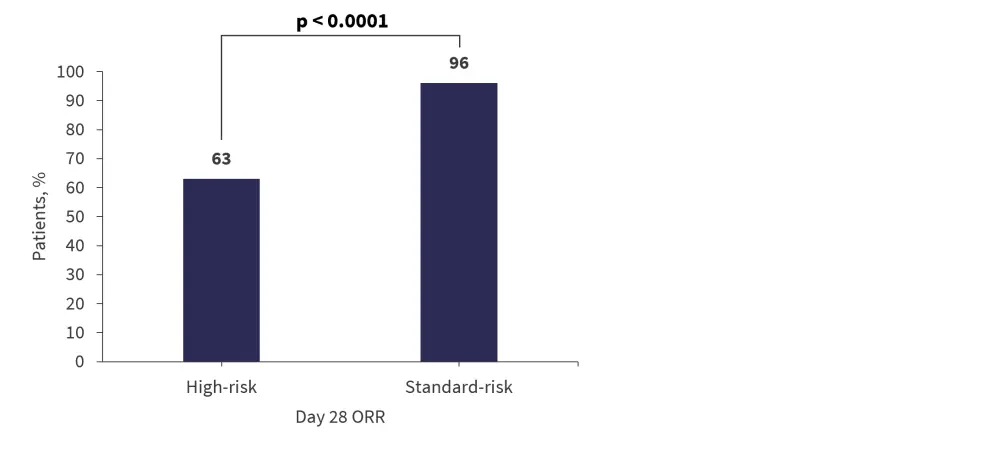
ORR, overall response rate.
*Adapted from Lupo-Stanghellini.1
Conclusion
Results from this study validate the accuracy of using the Minnesota risk score as a tool for predicting Day 28 overall response rate, 2-year overall survival probability, and TRM in standard- and high-risk patients with aGvHD following PTCy. The authors suggested that this may be a better approach for identifying high-risk patients than using initial GvHD grade, allowing for more effective therapy.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?



