All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
Significance of patient and transplant factors in development of kidney dysfunction in patients with cGvHD
Allogeneic hematopoietic stem cell transplant (allo-HSCT) is a potentially curative therapy for hematologic malignancies1; however, use of allo-HSCT can lead to long term complications, such as chronic graft-versus-host disease (cGvHD) and kidney dysfunction, both of which can cause significant morbidity.1
Kidney dysfunction can present as acute kidney injury, which causes a drop from baseline in the estimated glomerular filtration rate (eGFR), and chronic kidney disease (CKD), which is a persistent drop in eGFR over 3 months or more.1 Individuals who have undergone allo-HSCT and develop CKD are at a higher risk of death compared with those individuals with normal eGFR. In addition, cGvHD is a risk factor for development of CKD.
Here, we summarize key findings from a study investigating the incidence of kidney dysfunction in patients with cGvHD and assessing the impact of kidney dysfunction on overall survival.1
Study design1
- Overall, 365 patients were included for analysis in the Clinical and Biological Factors Determining Outcomes in Chronic Graft-Versus-Host Disease (NCT00092235) study.
- Patients received multi-disciplinary evaluation for 1 week
- eGFR was calculated using patient age, sex, and serum creatinine
- Univariate and multivariate analysis was performed to investigate which factors were associated with kidney dysfunction
Results1
Patient and cGvHD characteristics at enrollment are shown in Table 1. The majority of patients were white and had received a human leukocyte antigen matched transplant.
Table 1. Baseline patient and cGvHD characteristics*
|
cGvHD, chronic graft-versus-host disease; HLA, human leukocyte antigen; NIH, National Institutes of Health. |
|
|
Characteristic, % unless otherwise stated |
All patients (N = 365) |
|---|---|
|
Median age (range), years |
49 (18.1–75) |
|
Sex |
|
|
Male |
44 |
|
Female |
56 |
|
Race |
|
|
Non-Hispanic White |
88 |
|
Non-Hispanic Black |
4 |
|
Hispanic other |
4 |
|
Hispanic White |
2 |
|
Asian |
1 |
|
Non-Hispanic other |
<1 |
|
HLA match |
|
|
Matched |
84 |
|
Mismatched |
13 |
|
Unknown |
2 |
|
Conditioning regimen |
|
|
Myeloablative |
55 |
|
Non-myeloablative |
44 |
|
Unknown |
1 |
|
Median time from transplant to cGvHD diagnosis (range), months |
7.8 (0.6–260.7) |
|
NIH Global Score |
|
|
Mild |
2 |
|
Moderate |
25 |
|
Severe |
73 |
|
Prior lines of systemic therapy |
|
|
0–2 |
27 |
|
3–5 |
54 |
|
6–8 |
16 |
|
9–10 |
2 |
|
Unknown |
<1 |
In this study, kidney dysfunction was defined as eGFR of <60 ml/min/1.73 m2, with moderate-severe kidney dysfunction defined as eGFR <45 ml/min/1.73 m2. For the study population, the median eGFR was 96.4 ml/min/ 1.73 m2, with kidney dysfunction occurring in 18% of patients and moderate-severe kidney dysfunction occurring in 8% of patients.
Univariate analysis
Univariate analysis revealed that increasing patient age was strongly associated with kidney dysfunction. Associations between other patient and transplant factors with kidney dysfunction is shown in Figure 1.
Figure 1. Associations between key patients and transplant factors with kidney dysfunction*
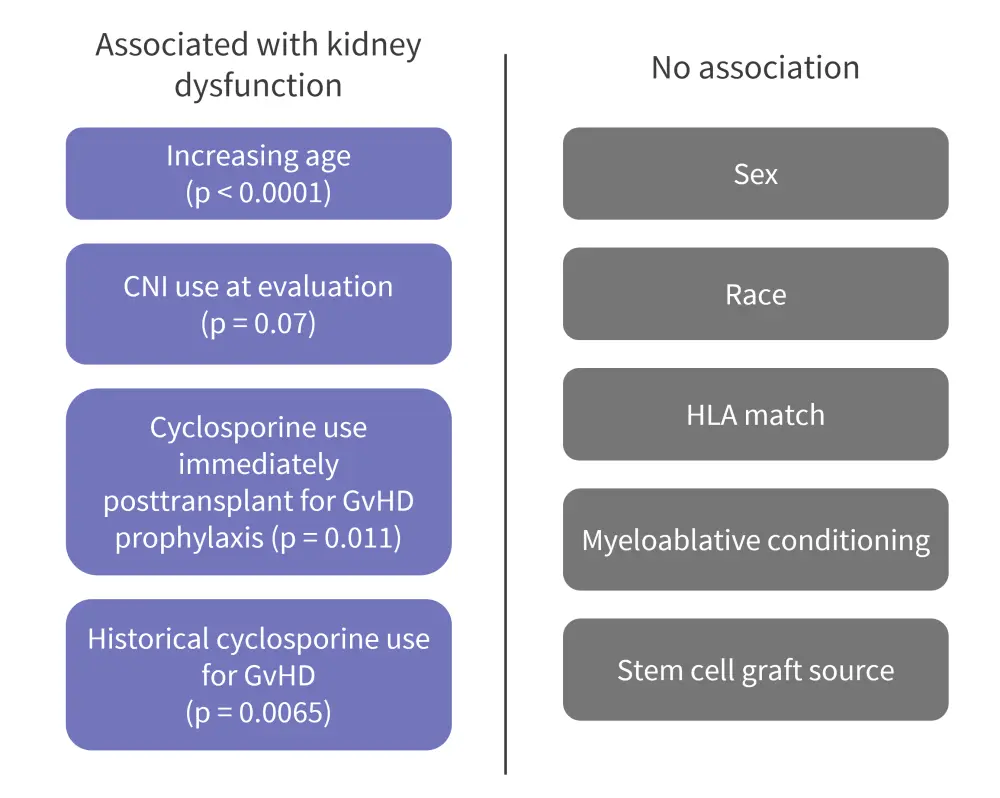
CNI, calcineurin inhibitor; GvHD, graft-versus-host disease; HLA, human leukocyte antigen.
*Adapted from Beshensky, et al.1
Other factors which were found to be associated with kidney dysfunction were:
- No/mild cGvHD involvement of joints/fascia (p = 0.009), mouth (p = 0.037), and skin (p = 0.03); these were more frequently moderate-severe in patients without kidney dysfunction.
- Presence of (p = 0.049) and/or increase in severity of proteinuria (p = 0.023) and increasing blood urea nitrogen (p < 0.0001).
- Presence of non-active GvHD (p = 0.04).
The average National Institutes of Health cGvHD organ score was lower in patients with kidney dysfunction (p = 0.0048). No association was found with diabetes (as measured by use of diabetes medication).
Overall survival
Median overall survival was found to be significantly lower in patients with moderate-severe kidney dysfunction versus those without, as shown in Figure 2. However, there were no significant differences in overall survival between patients with or without kidney dysfunction.
Figure 2. Median overall survival*
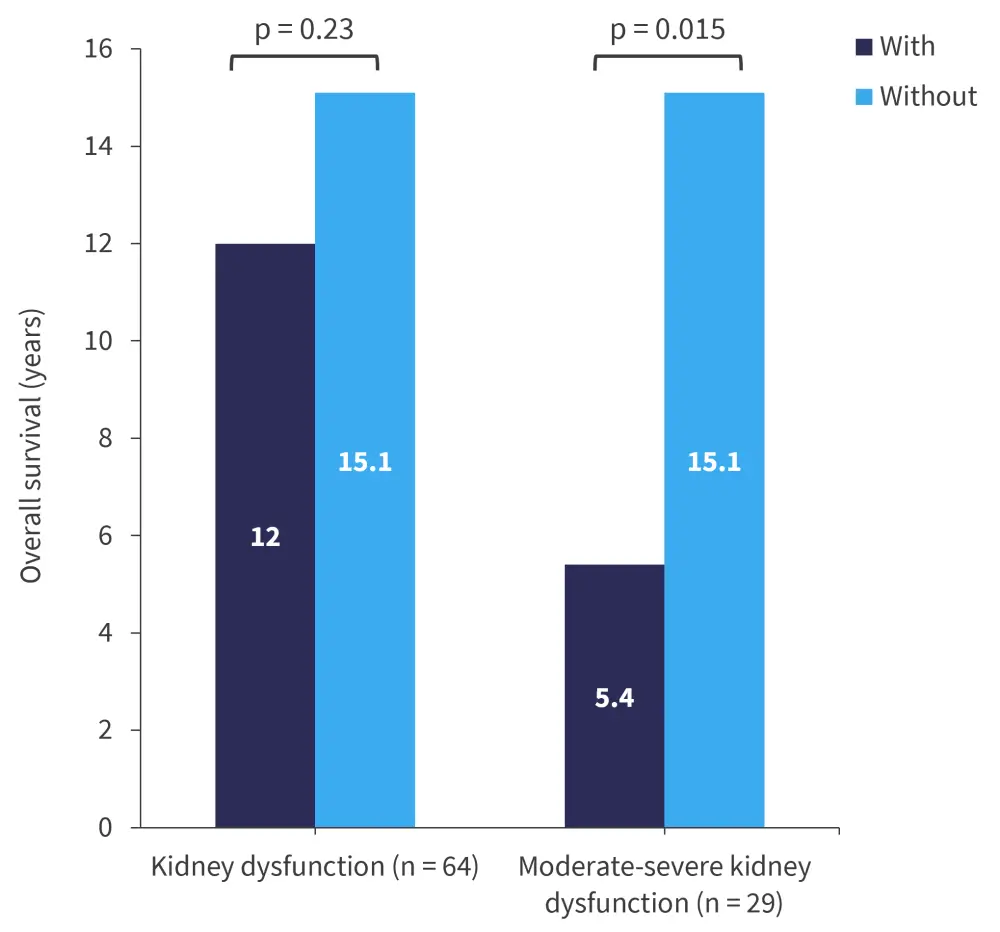
*Data from Beshensky, et al.1
Conclusion
This study revealed that approximately one fifth of patients with cGvHD had kidney dysfunction, with around half experiencing moderate-severe dysfunction; overall survival was significantly reduced in these patients. Certain factors, such as age and prior treatments, may have prognostic value for the development of kidney dysfunction in patient with cGvHD.
This study is limited by its cross-sectional design and measurement of eGFR at only a single time point. In addition, there were no control patients without cGvHD at a similar time point posttransplant. Therefore, additional multicenter, longitudinal studies are needed to fully determine the relationship between cGvHD, allo-HSCT, and kidney dysfunction.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?

