All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
Significance of DBY-HLA class II complexes in cGvHD development post-HSCT
Alloantibodies target Y-chromosome-encoded H-Y antigens, which are a group of minor histocompatibility antigens. One of these H-Y antigens, DBY, has been described after allogeneic hematopoietic stem cell transplant (HSCT) in male patients with a female donor. Previous studies in this patient group have suggested that presence of H-Y antibodies can be linked to disease remission. Furthermore, presence of plasma IgG antibodies against H-Y antigens at 3 months post-allo-HCT can be predictive of chronic graft-versus-host disease (cGvHD). However, the exact mechanisms by which H-Y antigens can correlate with GvHD are unknown; they are mainly expressed intracellularly in male reproductive organs and in the heart, which are not organs often affected by GvHD.
This study examined male patients who received HSCT from a female donor and investigated the significance of DBY and human leukocyte antigen (HLA) in cGvHD development.
Study design
Patients were included if they
- were ≥18 years of age;
- received a HLA-identical sibling donor graft between 2001 and 2019;
- achieved neutrophil engraftment; and
- had survived for ≥100 days.
Patient data was obtained from the Transplant Registry Unified Management Program, a Japanese national database of HCT data.
Human plasma, skin biopsy, and leukemia cell samples were obtained from the Jichi Medical University Hospital, Shimotsuke, and Jichi Medical University Saitama Medical Center, Saitama, JP. The method of H-Y antigen transfection is shown in Figure 1.
Figure 1. Transfection of H-Y antigens and HLA alleles*
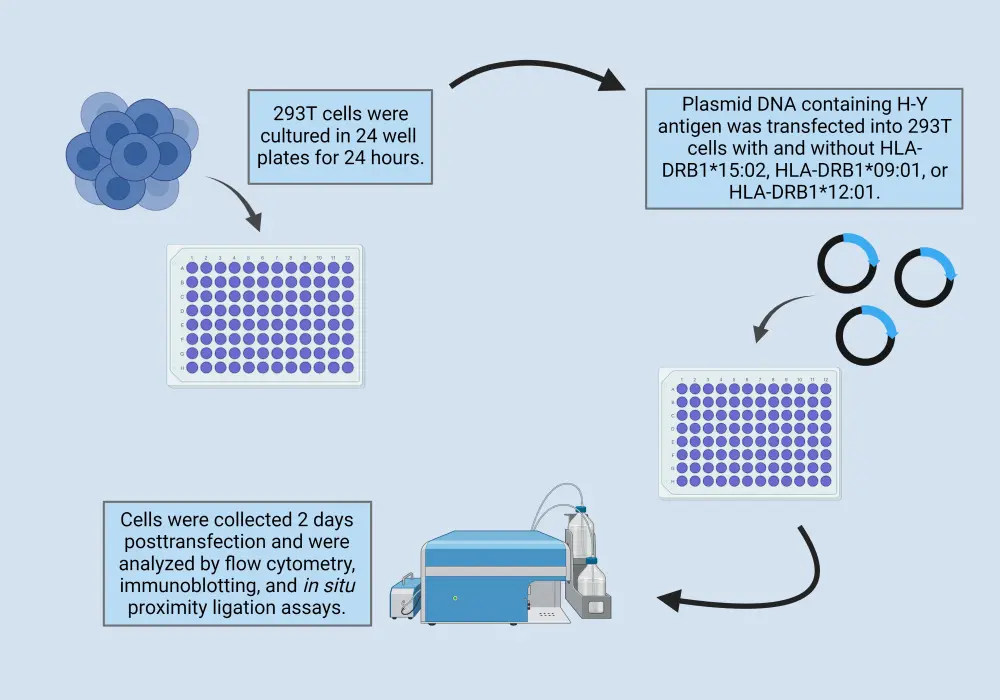
HLA, human leukocyte antigen.
*Data from Umino, et al.1 Created with Biorender.com
Results
Significance of HLA class II alleles
Multivariate analysis revealed that patients who were positive for HLA-DRB1*15:02 were at significantly higher risk of developing cGvHD (p = 0.025) and had a higher cumulative incidence of cGvHD than those who were negative; however, patients positive for HLA-DRB1*09:01 had a significantly lower risk of developing cGvHD (p = 0.010). Patients who were positive for HLA-DRB1*12:01 were not found to have a significantly higher or lower risk of developing cGvHD. The cumulative incidence of aGvHD (Grade II-IV) was similar between the HLA-DR positive and negative groups, suggesting this did not influence the rate of cGvHD.
In analysis of male-to-male HSCT, HLA-DR alleles had no influence on the incidence of cGvHD but did exhibit a lower cumulative incidence of cGvHD than the female-to-male cohort, suggesting that HLA-DR alleles are more influential in female-to-male HSCT.
Significance of DBY antigen
DBY is a model H-Y antigen and presence of DBY antibodies in plasma has proven a strong predictor of cGvHD. Cell surface expression testing revealed that DBY, in a full-length form, is expressed on the cell surface and forms complexes with HLA-DRB1*15:02. Additionally, plasma IgG antibody levels in patients with cGvHD were higher for antibodies against DBY/HLA-DRB1*15:02 complexes, compared to HLA-DRB1*15:02 alone. This suggests that DBY/HLA complexes cause a specific antibody response in cGvHD.
Plasma samples from 73 patients who received female-to-male HSCT were analyzed to determine if these antibodies can increase a patient’s risk of developing cGvHD. Of these patients, 43.8% were positive for anti-DBY/HLA class II complex antibodies, with the cumulative incidence of cGvHD higher in patients positive vs negative for these antibodies at 1 year (Figure 2).
Figure 2. Cumulative incidence of cGvHD at one year*
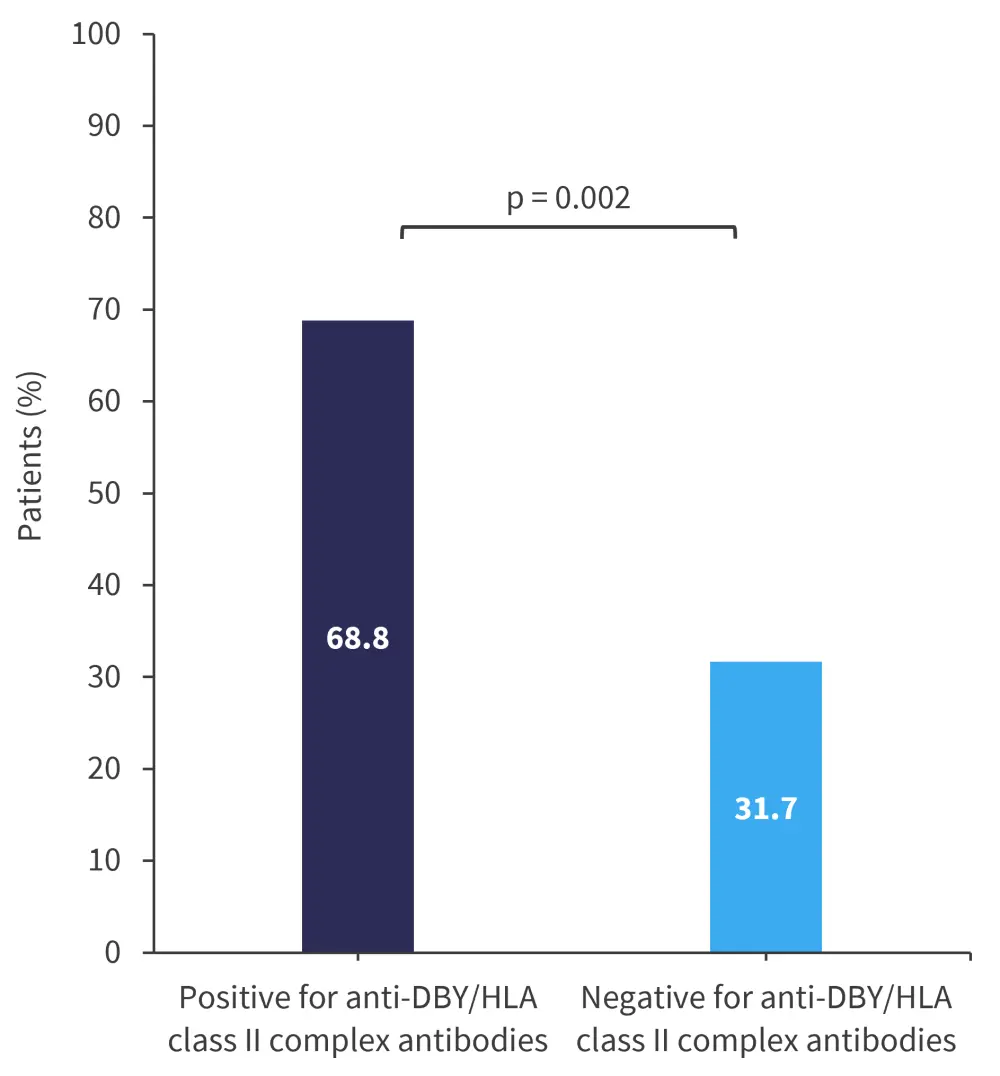
cGvHD, chronic graft-versus-host disease; HLA, human leukocyte antigen
*Data from Umino, et al.1
Expression of DBY/HLA complexes
Skin biopsy samples of female-to-male patients after HSCT were tested with immunohistochemistry staining for the presence of DBY and HLA class II in vascular endothelial cells. Staining was positive for the presence of both DBY and HLA. Expression levels in leukemic cells were also assessed and, in six male-derived leukemic cell lines which expressed HLA-DR, DBY was expressed at a similar level in all cells except human erythroleukemia cells.
Conclusion
The results of this study demonstrate that both HLA class II and DBY are influential in the risk of cGvHD after female-to-male HSCT. DBY and HLA class II were identified in vascular endothelial cells and leukemia cells, which can act as targets for alloantibodies. Cumulative incidence of cGvHD at 1 year was higher in patients who were positive for DBY-HLA class II complex antibodies, compared to those without. However, the specific HLA-DR present was shown to influence cGvHD development, with patients positive for HLA-DRB1*09:01 having a significantly lower risk of developing cGvHD and those who were positive for HLA-DRB1*15:02 at significantly higher risk of developing cGvHD.
Additional investigations of alloantigen-HLA complexes could assist in describing the complex pathophysiology of cGvHD and may lead to the development of new therapies.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?

