All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
GRAVITAS-119: A phase I trial of itacitinib plus calcineurin inhibitor-based regimens for GvHD prophylaxis
Despite prophylactic measures, graft-versus-host disease (GvHD) remains a serious complication of allogeneic hematopoietic cell transplant (HCT). Janus kinase (JAK) signaling plays a key role in the pathogenesis of GvHD, and JAK inhibition is being actively pursued as a therapeutic option for steroid-refractory patients.
Itacitinib is a JAK1 inhibitor that has been investigated in combination with corticosteroids for the treatment of GvHD, although the combined regimen did not improve overall response rates in the phase III GRAVITAS-301 trial. The phase I GRAVITAS-119 study (NCT03320642) evaluated itacitinib in combination with calcineurin inhibitor (CNI)-based regimens for the prophylaxis of GvHD. Here, we are pleased to summarize the results presented by Hannah Choe and colleagues during the 62nd American Society of Hematology (ASH) Annual Meeting and Exposition.1
GRAVITAS-119 study design1
GRAVITAS-119 is a single-arm, open-label, phase I study of itacitinib in combination with CNI-based regimens for prophylaxis of GvHD in adult patients undergoing allogeneic HCT for a hematologic malignancy. Enrolled patients were candidates for reduced-intensity conditioning and peripheral blood stem cell transplant. Other eligibility criteria included a Karnofsky score of ≥70% or ECOG score 0–2.
The primary endpoint was hematologic recovery at Day 28, defined by absolute neutrophil count (ANC) ≥500/mm3 and platelet count ≥20,000/mm3.
Secondary endpoints were GvHD-free, relapse-free survival (GRFS), transplant-related mortality, overall survival (OS), time to engraftment, incidence of GvHD, and safety.
The study design is shown in Figure 1.
Figure 1. Overview of GRAVITAS-119 study design1
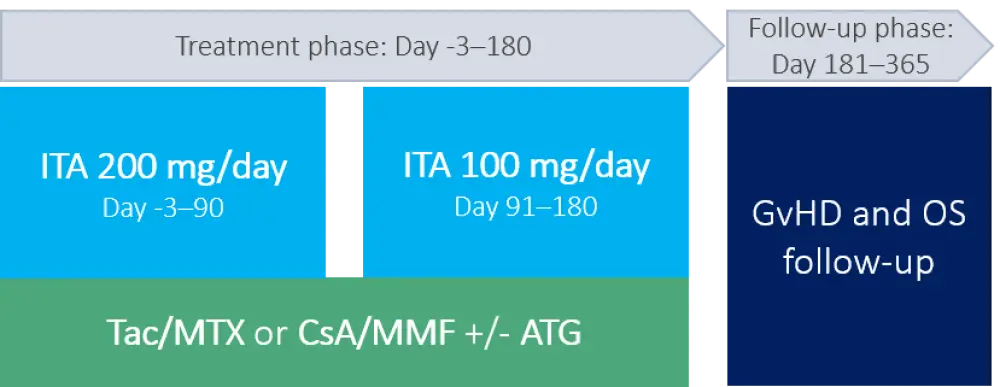
ATG, anti-thymocyte globulin; CsA, cyclosporine A; ITA, itacitinib; MMF, mycophenolate mofetil; MTX, methotrexate; OS, overall survival, Tac, tacrolimus.
Patient disposition and characteristics
- For the 65 patients treated with itacitinib, the CNI-based regimen used was tacrolimus (Tac)/methotrexate (MTX) in 41 patients (with anti-thymocyte globulin [ATG]: 8; without ATG: 33), and cyclosporine A (CsA)/mycophenolate mofetil (MMF) in 24 patients (with ATG: 16; without ATG: 8).
- While 73.8% of patients received itacitinib for > 90 days (median exposure 140 days), the majority of patients discontinued treatment before Day 180 (73.2% in the itacitinib + Tac/MTX arm, 50.0% in the itacitinib + CsA/MMF arm).
- The most common reasons for itacitinib discontinuation were adverse events (21.5%) and relapse (16.9%).
Selected characteristics for patients receiving itacitinib plus CNI-based regimen, with or without ATG, are shown in Table 1.
- The most common underlying malignancy was acute myeloid leukemia (40%).
- Two-thirds of patients had an intermediate risk score.
- Half of transplant donors were matched related, and 40% were matched unrelated.
- The most common conditioning regimen was busulfan/fludarabine (50%), followed by fludarabine/melphalan (18%).
Table 1. Selected patient and transplant characteristics1
|
ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; ATG, anti-thymocyte globulin; ECOG, Eastern Cooperative Oncology Group; HLA, human leukocyte antigen; MDS, myelodysplastic syndromes. |
||
|
|
Without ATG |
With ATG |
|---|---|---|
|
Patient characteristic |
||
|
Median age, years (range) |
65 (25–76) |
64 (42–72) |
|
ECOG grade, % |
|
|
|
Underlying malignancy, % |
|
|
|
Disease risk index, % |
|
|
|
Transplant characteristic |
||
|
HLA donor type, % |
|
|
Hematologic recovery
- All patients achieved both neutrophil and platelet recovery (Table 2).
- Hematologic recovery was achieved at the Day 28 primary endpoint in 64 out of 65 patients; one patient with myelofibrosis achieved ANC recovery on Day 31.
Table 2. Hematologic recovery1
|
ANC, absolute neutrophil count; CsA, cyclosporine A; ITA, itacitinib; MMF, mycophenolate mofetil; MTX, methotrexate; Tac, tacrolimus. |
|||
|
|
ITA + Tac/MTX |
ITA + CsA/MMF |
Total |
|---|---|---|---|
|
ANC recovery* |
|
|
|
|
Evaluable‡, n |
38 |
23 |
61 |
|
Platelet recovery† |
|
|
|
|
Evaluable‡, n |
23 |
16 |
39 |
Graft failure
Secondary graft failure occurred in two patients, both of whom received a second transplant. One graft failure occurred on treatment, at Day 65, the other at Day 182 during follow-up, approximately 4 months after the last itacitinib dose.
GvHD, relapse, and survival outcomes
Outcomes for secondary endpoints are summarized in Table 3.
- Rates of acute GvHD compared favorably with historical data for CNI-based regimens.
- For patients receiving ATG-containing regimens, cumulative incidence of moderate or severe chronic GvHD and of relapse at 1 year were lower, and 1-year GRFS rate was higher, compared with patients not receiving ATG.
Table 3. Secondary endpoints1
|
ATG, anti-thymocyte globulin; GRFS, GvHD-free and relapse-free survival; GvHD, graft-versus-host disease; OS, overall survival. |
||
|
Endpoint, % |
Without ATG |
With ATG |
|---|---|---|
|
Acute GvHD, cumulative incidence at Day 180 |
|
|
|
Chronic GvHD, cumulative incidence at 1 year |
|
|
|
Relapse or progression, cumulative incidence at 1 year |
28.2 |
4.3 |
|
Estimated GRFS at 1 year |
23.1 |
60.9 |
|
Estimated OS at 1 year |
74.3 |
82.6 |
Adverse events
- The most common hematologic adverse events leading to itacitinib dose modification/discontinuation were thrombocytopenia (9.2%), mixed chimerism (6.2%), and neutropenia (3.1%).
- Other common non-hematological Grade ≥3 side effects were diarrhea (15.4%), hypertension (13.8%), and hypertriglyceridemia (12.3%).
- Grade ≥3 infections occurred in 33.3% of patients receiving ATG-containing regimens, and 26.8% of patients not receiving ATG.
- Cytomegalovirus (CMV) infection of any grade occurred in 16.9% of patients; all cases had donor- and/or recipient-positive CMV serostatus.
- Primary cause of death on treatment was infection (two patients), and primary causes of death during follow-up were disease relapse (five patients) and infection (three patients).
Conclusion
The addition of itacitinib to CNI-based regimens was well tolerated, with 64 out of 65 patients achieving the primary endpoint of hematologic recovery within 28 days. While the incidence of acute GvHD was low and 1-year GRFS rates were encouraging, treatment appeared to have little impact on the frequency of chronic GvHD, except for patients receiving ATG.
Larger and more homogeneous study cohorts are required to further evaluate the efficacy of this combination for GvHD prophylaxis. Evaluation of an itacitinib + post-transplant cyclophosphamide combination is currently underway in the GRAVITAS-119 trial.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?

