All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
Effects of antibiotic exposure following allo-HCT with non-myeloablative Flu-TBI conditioning
Antibiotics play a significant role in acute gastrointestinal graft-versus-host disease (GI-GvHD) following allogeneic hematopoietic cell transplantation (allo-HCT). Antibiotic use can negatively impact microbial diversity and exacerbate GI-GvHD, resulting in higher rates of non-relapse mortality and worse overall survival (OS) outcomes in patients.
Most current data on the use of antibiotics in HCT are limited to the setting of reduced intensity conditioning and myeloablative HCT, with a lack of data from non-myeloablative (NMA) HCT. Understanding the effects of antibiotic exposure is important in the NMA HCT setting, where mucosal barrier integrity is less compromised compared with reduced intensity conditioning and myeloablative HCT, allowing for a focused analysis of the sole impact of antibiotic use on GI-GvHD and HCT outcomes.
Van Groningen et al. recently published an article in Leukemia & Lymphoma on the impact of antibiotic exposure on GI-GvHD following allo-HCT with NMA conditioning. Here, we summarize their findings.
Methods1
-
This was a single-center retrospective analysis that included patients who received allo-HCT following fludarabine/higher total body irradiation (Flu-TBI) -based NMA conditioning for a hematologic malignancy.
-
Flu-TBI conditioning consisted of 30 mg/m2 fludarabine on Days −4, −3, and −2, and low-dose TBI on Day −1.
-
In the event of mismatched unrelated donor transplant, patients received additional in vivo T cell depletion with 2 mg/kg/day rabbit-ATG on Days −8, −7, −6, and −5.
-
Antibiotics received by patients included ciprofloxacin, ceftazidime, meropenem, ceftazidime, metronidazole, and valacyclovir.
-
Key outcome measures included non-relapse mortality (NRM), relapse-free survival (RFS), OS, and GvHD relapse-free survival (GRFS).
Key findings1
-
A total of 150 patients were included that had received Flu-TBI-based NMA conditioning.
-
Median patient age was 59 years and 53% were male.
-
Antibiotic exposure occurred in 60% of patients, with 40% receiving prophylactic ciprofloxacin, and 20% receiving broad-spectrum antibiotics.
-
NRM at 1 year was 19% in patients who received antibiotics, and 10% in those who did not.
-
OS and RFS were not significantly affected by antibiotic exposure.
-
GRFS was significantly lower in patients receiving antibiotics vs those who did not (42% vs 55%).
-
Antibiotic exposure was shown to play a significant role in the occurrence of GvHD (Figure 1).
Figure 1. Incidence of acute and chronic GvHD by antibiotic exposure status*
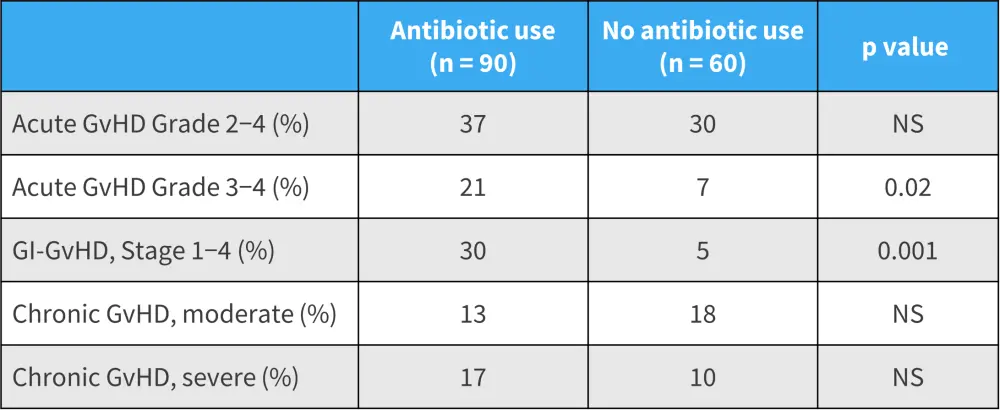
GvHD, graft-versus-host disease; NS, not significant.
*Data from Van Groningen, et al.1
|
Key learnings |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?


