All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
Diverting enterostomy to treat steroid-resistant gastrointestinal acute graft-versus-host disease
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a curative therapy for a variety of hematologic malignancies; however, up to 50% of recipients develop acute graft-versus-host disease (aGvHD). aGvHD involving the gastrointestinal (GI) tract (GI-aGvHD) is difficult to treat, and in its most severe forms it carries a mortality rate of >95%. Any part of the GI tract may be affected, but the ileum is most commonly involved due to its high density of lymphoid follicles.
Surgical intervention in patients with GI-aGvHD is usually restricted to emergency presentations such as bowel perforation, GI hemorrhage, and intestinal necrosis. However, Justine Khodr et al., in Annals of Surgery,1 hypothesize that a proximal diverting enterostomy (DE), a procedure in which the bowel is brought out to the abdominal surface to form a stoma,2 could improve management of severe steroid-refractory GI-aGvHD in the distal excluded ileocolonic segment. The procedure diverts fecal matter away from the affected bowel, reducing bacterial translocation (the passage of bacteria through gut mucosa to normally sterile tissues3), which is implicated in GI-aGvHD pathophysiology. The results of their retrospective study are summarized in this article.
Study design
- Patients with steroid-refractory Stage III or IV GI-aGvHD who had undergone allo-HSCT between August 2004 and December 2018 were identified, as shown in Figure 1.
- Imaging of the GI tract (upper and lower digestive endoscopy, video-capsule endoscopy and/or computed tomography (CT), and barium meal follow-through) and plasma citrulline were used to assess the extent and severity of intestinal damage.
- DE was not offered to patients considered too frail for surgery.
Figure 1. Identification of patients for inclusion*
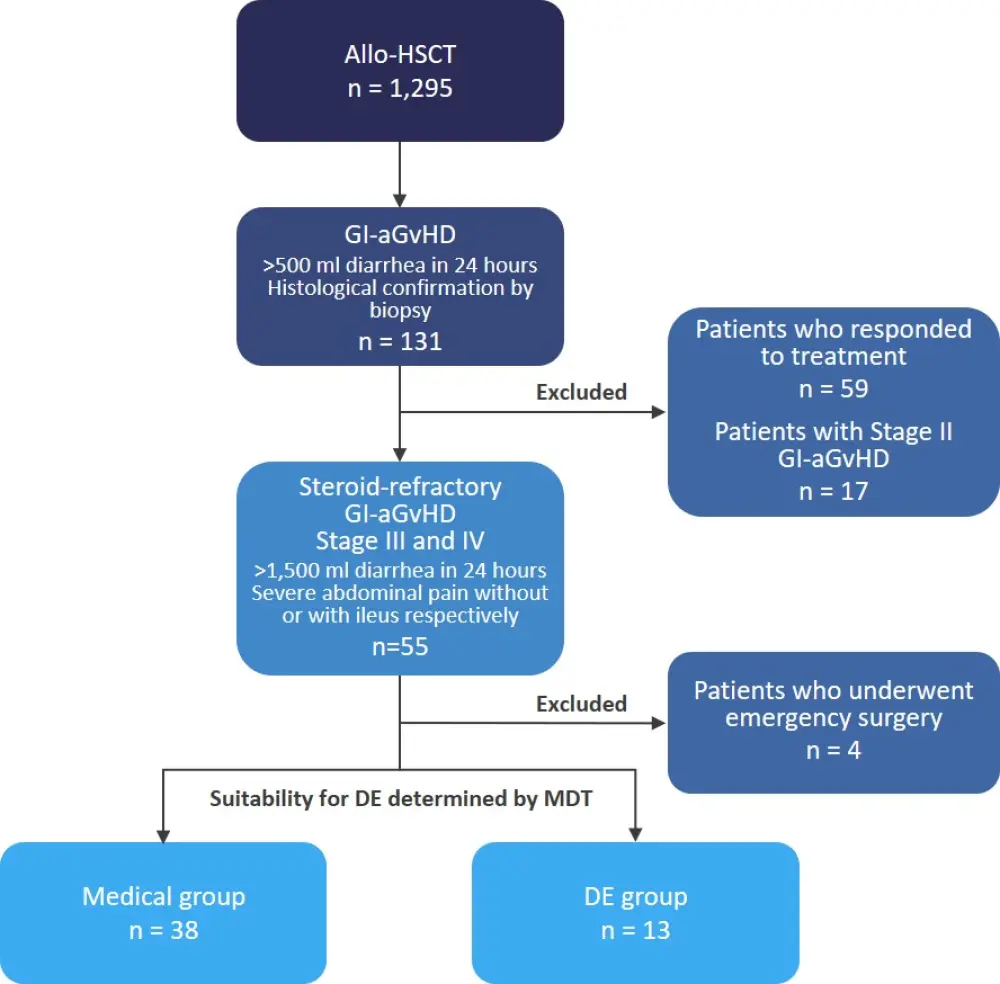
allo-HSCT, allogeneic hematopoietic stem cell transplant; DE, diverting enterostomy; GI-aGvHD, acute graft-versus-host disease involving the gastrointestinal tract; MDT, multidisciplinary team.
*Adapted from Khodr, et al.1
Baseline characteristics
Patient characteristics, presented in Table 1, did not differ significantly between the medical group and the DE group, except for cytomegalovirus status, which was significantly higher in the DE group (p = 0.003).
Table 1. Patient characteristics and transplantation modalities*
|
ALL, acute lymphoblastic leukemia; AML, acute myelogenous leukemia; CLL, chronic lymphocytic leukemia; CML, chronic myelogenous leukemia; CMV, cytomegalovirus; DE, diverting enterostomy; HL, Hodgkin lymphoma; IQR, interquartile range, MDS, myelodysplastic syndrome; MM, multiple myeloma; MPD, myeloproliferative disorder; NHL, non-Hodgkin lymphoma. |
||
|
Characteristic, % (unless otherwise stated) |
Medical group |
DE group |
|---|---|---|
|
Median age, years (IQR) |
54.5 (41.0–60.0) |
44.0 (38.0–49.0) |
|
Female |
36.8 |
53.8 |
|
Hematologic malignancy |
|
|
|
MM |
13.2 |
23.1 |
|
ALL |
2.6 |
30.8 |
|
HL |
0.0 |
7.7 |
|
NHL |
15.8 |
0.0 |
|
AML |
31.6 |
15.4 |
|
MDS |
0.0 |
7.7 |
|
CLL |
10.5 |
0.0 |
|
MPD |
15.8 |
15.4 |
|
CML |
10.5 |
0.0 |
|
Prophylactic digestive decontamination |
44.1 |
69.2 |
|
Positive recipient CMV serology |
31.6 |
69.2 |
|
Median plasma citrulline, mmmol/L (IQR)† |
26 (19–32) |
27 (17–33) |
Characteristics of aGvHD, presented in Table 2, were comparable between both groups, with the exception of a significantly higher rate of proximal GI-aGvHD involving the jejunum in the medical treatment group (p < 0.0001).
Table 2. Characteristics of aGvHD*
|
aGvHD, acute graft-versus-host disease; DE, diverting enterostomy; GI-aGvHD, aGvHD involving the gastrointestinal tract; ICU, intensive care unit; IQR, interquartile range. |
||
|
Characteristic, % (unless otherwise stated) |
Medical group |
DE group |
|---|---|---|
|
GI-aGvHD stage |
|
|
|
Stage 3 |
28.9 |
23.1 |
|
Stage 4 |
71.1 |
76.9 |
|
Proximal GI-aGvHD (involving jejunum)† |
74.9 |
7.7 |
|
Liver aGvHD stage |
|
|
|
No damage |
65.8 |
69.2 |
|
Stage 1 |
0.0 |
7.7 |
|
Stage 2 |
2.6 |
0.0 |
|
Stage 3 |
10.5 |
7.7 |
|
Stage 4 |
21.1 |
15.4 |
|
Skin aGvHD stage |
|
|
|
No damage |
34.2 |
46.2 |
|
Stage 1 |
18.4 |
7.7 |
|
Stage 2 |
18.4 |
30.8 |
|
Stage 3 |
18.4 |
7.7 |
|
Stage 4 |
10.5 |
7.7 |
|
No. of immunosuppressor lines |
|
|
|
n = 1 |
8.8 |
0.0 |
|
n = 2 |
38.2 |
61.5 |
|
n = 3 |
35.3 |
30.8 |
|
n = 4 |
17.6 |
0.0 |
|
n = 5 |
0.0 |
7.7 |
|
Missing data |
10.5 |
0.0 |
|
ICU stay during hospitalization |
65.6 |
76.9 |
|
Median delay from transplantation to aGvHD, days (IQR) |
30 (25–52) |
30 (27–40) |
|
Median plasma citrulline during aGvHD, mmmol/L (IQR) |
4 (3–6) |
3 (3–5) |
Results
- Overall survival was significantly higher in the DE group, as shown in Table 3.
- DE reduced the risk of death (hazard ratio, 0.226; 95% confidence interval, 0.092–0.554; p = 0.0011).
- Lower infection-related cause of death was seen in the DE group (30.8%) vs the medical group (57.9%), although this did not reach statistical significance (p = 0.091).
- Both groups showed a dramatic decrease in citrulline levels when measured at the worst clinical intensity of GI-aGvHD.
Table 3. Overall survival and causes of death*
|
DE, diverting enterostomy; GI, gastrointestinal; OS, overall survival. |
||
|
Outcome, % |
Medical group |
DE group |
|---|---|---|
|
1-year OS |
5 |
54 |
|
2-year OS |
2.5 |
31 |
|
Cause of death |
|
|
|
Relapse |
2.9 |
10 |
|
Hemorrhage (non-GI) |
10.5 |
0 |
|
Pneumonia |
22.9 |
20 |
|
Encephalitis |
2.8 |
0 |
|
Staphylococcal sepsis |
2.8 |
0 |
|
Liver failure |
5.7 |
20 |
|
Heart failure |
5.7 |
10 |
|
Respiratory failure |
5.7 |
20 |
|
Kidney failure |
5.7 |
10 |
|
GI complications |
45.7 |
30.8 |
|
Obstruction |
5.7 |
0 |
|
GI sepsis |
34.3 |
20 |
|
GI hemorrhage |
5.7 |
20 |
|
Overall infections |
57.9 |
30.8 |
Severe postoperative complications occurred in three patients in the DE group, with one patient having volvulus of enterostomy requiring endoscopic treatment, the second developing cellulitis with enterocutaneous fistula leading to death 25 days post-operation, and the third experiencing GI perforation leading to death 35 days post-operation.
In the medical group, ten patients were considered for surgery but received medical treatment only: three were considered too frail for surgery, one improved with medical treatment, and six patients should have undergone DE but did not and all six died within the first year after GI-aGvHD onset.
Conclusion
DE significantly improved survival outcomes in patients with steroid-refractory GI-aGvHD compared to medical management alone and this supports previous findings from a smaller study.1 The effectiveness of DE is further validated given the significantly higher rate of cytomegalovirus infection in the DE group, a well-recognized cause of mortality in GI-aGvHD. However, notable limitations of this study include the small sample size, retrospective nature, and the fact that DE was preferentially performed in patients with distal GI-aGvHD, meaning the two groups were not entirely comparable. Given the poor survival rate in the medical group combined with the dramatic drop in citrulline levels in both groups, indicating deep intestinal failure and risk of bacterial translocation, Khodr and colleagues propose that DE should be considered in steroid-resistant GI-aGvHD regardless of GI-aGvHD location; research to assess this is ongoing.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?

