All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The gvhd Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the gvhd Hub cannot guarantee the accuracy of translated content. The gvhd and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The GvHD Hub is an independent medical education platform, sponsored by Medac and supported through grants from Sanofi and Therakos. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View GvHD content recommended for you
Comparison of endoscopic and histological signs of aGvHD in the upper gastrointestinal tract
Allogenic hematopoietic stem cell transplantation (allo-HSCT) represents a potentially curative therapy for patients with high-risk hematological malignancies. Complications can occur when donor immune cells attack healthy recipient cells resulting in graft-versus-host disease (GvHD). Acute GvHD (aGvHD) commonly affects the gastrointestinal tract (GIT), with severe cases conferring an adverse prognosis.1
The symptoms of GIT aGvHD include nausea, vomiting, anorexia, and dyspepsia, with histological analysis of biopsies playing a vital role in diagnosis.2 The correlation between endoscopic and histological findings has not been well established for the upper GIT.2
Below, we summarize a recent article published by Kreft, et al.2 in Leukemia & Lymphoma evaluating the correlation between the histological diagnosis of aGvHD and endoscopic findings of the upper GIT.
Study design and patient characteristics
This retrospective analysis included 97 patients who received allo-HSCT between 2006 and 2019. The median age was 54 years and the median days after allo-HSCT was 113 days (Table 1). Biopsy specimens were assessed for histological signs of aGvHD using the Lerner scheme (Grade 0: normal epithelia; Grade 1: single-cell apoptosis; Grade 2: crypt destruction; Grade 3: focal epithelial loss; Grade 4: diffuse epithelial loss, denudation)3,4,5 and the adaptation for esophagus GvHD (Grade 0: normal epithelia; Grade 1: cytoplasmic vacuolization; Grade 2: single-cell apoptosis; Grade 3: separation of the stroma-epithelial junction; Grade 4: denudation).6
Table 1. Patient characteristics*
|
ALL, acute lymphoblastic leukemia; allo-HSCT, allogenic hematopoietic stem cell transplantation; AML, acute myeloid leukemia; BPDCN, blastic plasmacytoid dendritic cell neoplasm; HLA, human leucocyte antigen; MDS, myelodysplastic syndrome; MPN, myeloproliferative neoplasm. |
|
|
Characteristics, n (unless otherwise stated) |
N = 97 |
|---|---|
|
Male |
54 |
|
Median age (range), years |
51 (19–72) |
|
Median days after allo-HSCT (range), days |
113 (16–4,000) |
|
Disease |
|
|
AML |
47 |
|
MDS |
7 |
|
MDS/MPN |
2 |
|
MPN |
9 |
|
ALL |
7 |
|
Lymphoma |
211 |
|
Aplastic anemia |
3 |
|
BPDCN |
1 |
|
Donor type |
|
|
Sibling HLA-identical |
18 |
|
Unrelated HLA-identical |
50 |
|
Unrelated HLA-mismatch |
23 |
|
Unknown |
6 |
Results
Biopsy sites
Overall, 59 patients had biopsies from all four sites of the upper GIT (duodenum, antrum, corpus, and esophagus).
Three sites were biopsied in 20 patients:
- Antrum, corpus, and esophagus: 11
- Duodenum, antrum, and corpus: 8
- Duodenum, antrum, and esophagus: 1
Two sites were biopsied in 11 patients:
- Antrum and corpus: 6
- Duodenum and corpus: 2
- Duodenum and antrum: 1
- Corpus and esophagus: 1
- Duodenum and esophagus: 1
Only one site was biopsied in 7 patients:
- Antrum: 5
- Corpus: 1
- Esophagus: 1
Histological signs of GvHD
- Histological signs of GvHD were present in 48 patients
- The duodenum was the site with the most histological signs of aGvHD, with significantly more than in the corpus (p = 0.004) and antrum (p = 0.01)
- The esophagus had the second highest, with significantly more than the corpus (p = 0.001) and antrum (p = 0.005)
- There were no significant differences in histological signs between the corpus and antrum
- The correlation of histological aGvHD grades within different biopsy sites was poor (Fleiss’ kappa = 0.33)
- In terms of endoscopic findings, ulcers, erosion, atrophy, and white plaques were significantly associated with histological signs of aGvHD (Table 2)
- In some cases where endoscopic findings were present but there were no histological signs of aGvHD, histological signs of aGvHD were found in biopsies from other sites
- Signs of aGvHD outside the upper GIT were present in the skin (n = 53), lower GIT (n = 20), and liver (n = 11), of which 31, 20, and 4 patients had histological signs of GvHD in upper GIT biopsies
Table 2. Statistically significant association between histological and endoscopic findings*
|
GvHD, graft-versus-host disease. |
||||||
|
Site |
Endoscopic |
Histology GvHD |
||||
|---|---|---|---|---|---|---|
|
0 |
1 |
2 |
3 |
4 |
||
|
Esophagus |
All |
38 |
14 |
14 |
8 |
2 |
|
White |
2 |
1 |
— |
3 |
— |
|
|
Corpus |
All |
60 |
19 |
8 |
0 |
1 |
|
Ulcer† |
1 |
— |
2 |
— |
— |
|
|
Antrum |
All |
57 |
24 |
7 |
1 |
2 |
|
Ulcer† |
— |
1 |
— |
— |
1 |
|
|
Duodenum |
All |
30 |
27 |
6 |
3 |
6 |
|
Atrophy† |
— |
2 |
— |
— |
2 |
|
|
Erosion† |
— |
9 |
2 |
1 |
1 |
|
Survival outcomes
In total, 57 patients died (Figure 1). The mean observation period was 694 days (range, 31–7,576 days).
Histological signs of aGvHD in all four sites were significantly associated with overall mortality:
- Esophagus hazard ratio (HR): 2.0, 1.1–3.6; p = 0.02
- Corpus HR: 1.8, 1.0–3.1; p = 0.05
- Antrum HR: 2.0, 1.1–3.4, p = 0.01
- Duodenum HR: 2.2, 1.1–4.1; p = 0.02
The maximal Lerner grade of 2 (HR, 2.7, 1.0–7.33; p = 0.03) and having more than two sites with histological signs of aGvHD (HR, 3.1, 1.1–8.9; p = 0.055) had a significant effect on overall survival. Non-relapse mortality was significantly associated with histological signs of GvHD in the antrum (HR, 1.8, 1.1–3.2; p = 0.03) but not other locations, the number of sites involved, or the maximum Lerner grade.
Figure 1. Causes of death among patients*
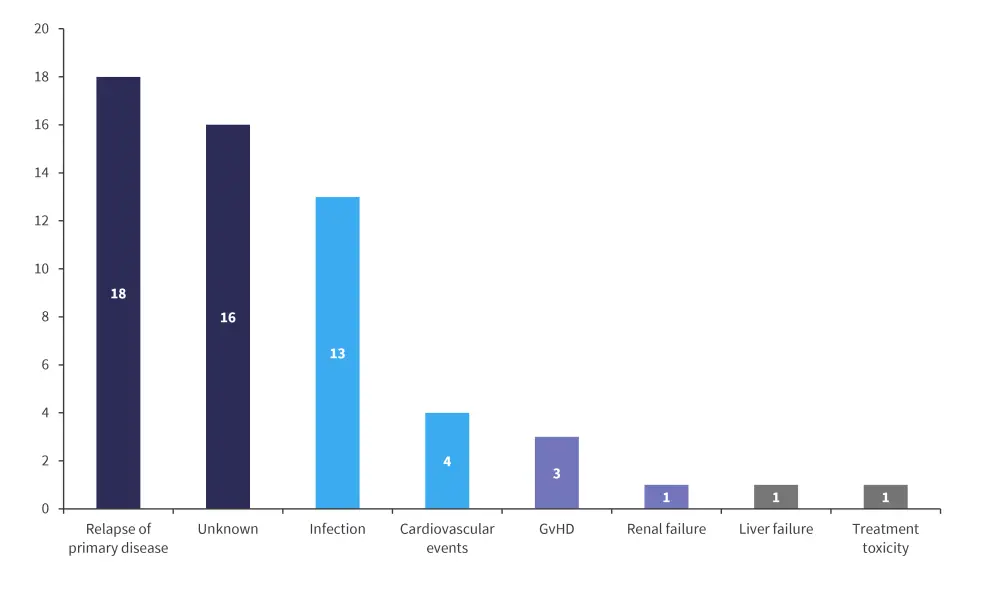
GvHD, graft-versus-host disease.
*Data from Kreft, et al.2
Conclusion
In this retrospective analysis across four sites, the duodenum and esophagus had the highest proportion of histological signs of aGvHD in the upper GIT, suggesting biopsies should focus on these two sites. Although the endoscopic findings of white plaques, ulcers, atrophy, and erosion were significantly associated with histological signs of aGvHD, there was also no correlation between endoscopic findings and histological signs of aGvHD for several patients.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
Which consideration most strongly guides your decision to escalate therapy in SR-aGvHD?

